Intraoperative Ultrasound
Home » Resources » Ultrasound-Guided Procedures » Intraoperative Ultrasound

History
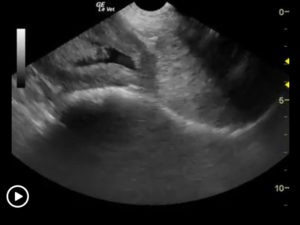
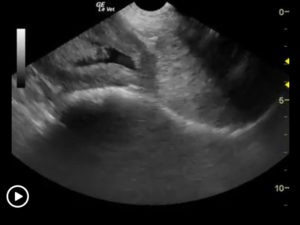
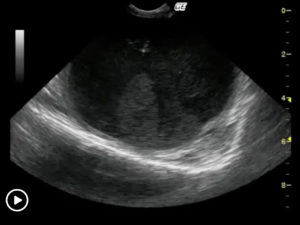
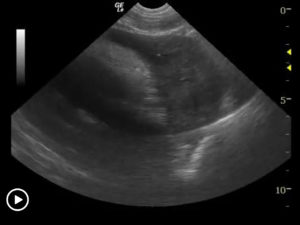
We developed this technique to be used on any abdominal organ but is especially effective in case of infiltrative, focal and multifocal GI lesions. The problem is that the surgeon cannot often see what the clinical sonographer is observing from a transabdominal sonographic perspective. If the organ serosa is not visibly affected, the surgeon will simply perform a “shopping spree” of intestinal biopsies as opposed to a precise sampling procedure of the most representative lesion that we observe sonographically. Hence we may identify and resect the most representative mural lesions with this method.
Procedure
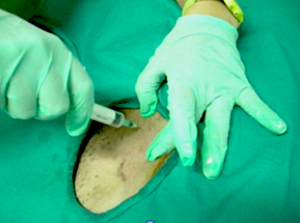
Acoustic gel is placed into a double surgical glove to keep the outside exposed glove sterile. Cold sterilize the ultrasound probe with alcohol before putting it in the glove. Pull the glove tight on top the probe to ensure adequate probe/gel/glove coupling occurs to avoid any air entrapment. Have the surgeon exteriorize the bowel or expose the target organ to be sampled. A technician pours saline on the bowel (or other organ) as a coupling agent. Scan the organ to define the most representative region of the mural pathology that was observed transabdominally. Then define the best healthy tissue where the infiltrative pattern or pathology subsides and resect the lesion at this identified point of healthy tissue proximal and distal to the affected region. This procedure should take the sonographer 10 minutes or so and the surgeon may do the rest.
Comments
This procedure ensures as complete a resection of unhealthy bowel as possible and also ensures that healthy bowel is utilized for the anastamosis. Postoperative dehiscence may be avoided by this intraoperative intervention. More on this technique may be seen in our abstract from ECVIM 2009 (Intraoperative Ultrasound for Precise Biopsy and Resection of Transabdominally Detected Intestinal Lesions in 3 cats. Lindquist, Casey, Frank)

More Ultrasound-Guided Procedures

Bubble Study
The reason to perform a bubble study is to confirm the presence of shunting of blood from venous to arterial flow such as a Reverse VSD or a Reverse PDA.

Gallbladder Motility Study
NPO overnight. Time 0 min: Measure GB in long axis and short axis from subxiphoid approach and right intercostal approach. The proper position is maximum

Lindquist Compression Technique For Thoracic FNA
This technique often makes inaccessible thoracic lesions accessible.
Traumatic Catheterization Procedure
Sedation Use largest open-end rigid polypropylene urinary catheter cut diagonally to create a sharp edge like a needle bevel. Lube heavily and pass catheter retrograde
UGELAB for Transitional Cell Carcinoma in the Dog
Dr. Dean Cerf, Ridgewood Veterinary Hospital NJ and Dr. Eric Lindquist, SonoPath.com For More Information Contact Dr. Dean Cerf at Ridgewood Veterinary Hospital, Ridgewood, NJ,

Ultrasound-Guided Lymph Node Culture
This type of lymph node sampling is helpful in determining infected lymph nodes vs. lymphoma. Supplies: 6 cc Luer lock syringe 1cc of saline 2
Ultrasound-Guided Pericardiocentesis
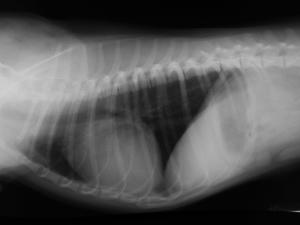
History Pericardial effusions typically cause some level of cardiomegaly on radiographs but note poor vascular volume in the pulmonary artery and vein. Muffled heart sounds

Ultrasound-Guided Sampling Procedures
Description Ultrasound-guided needle sampling is frequently used in the diagnostic evaluation of patients. Fine needle aspiration has the advantage of requiring minimal or no sedation
