Ultrasound-Guided Pericardiocentesis
Home » Resources » Ultrasound-Guided Procedures » Ultrasound-Guided Pericardiocentesis
History
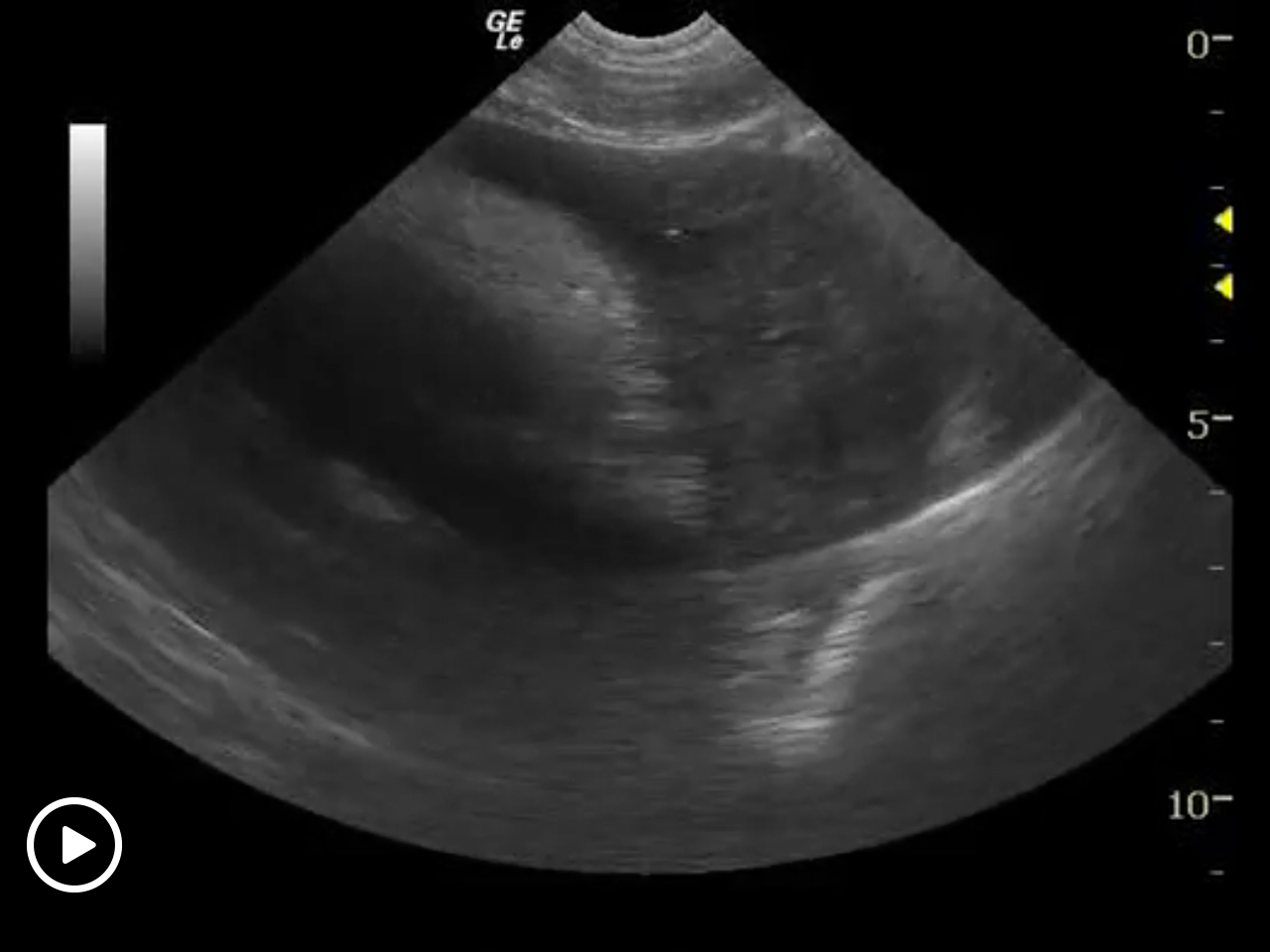
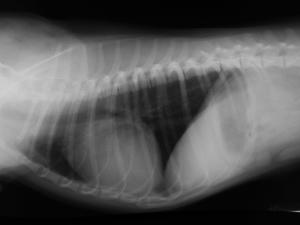
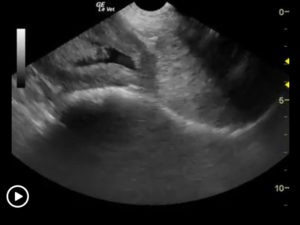
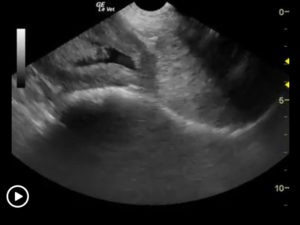
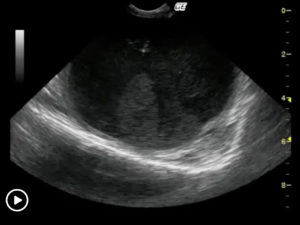
Pericardial effusions typically cause some level of cardiomegaly on radiographs but note poor vascular volume in the pulmonary artery and vein. Muffled heart sounds and electrical alternans on ECG may also be present. In this case the sonogram is quite direct and simple to diagnose while potential masses may be elusive. In order to provide immediate relief from the tamponade effect from pericardial effusion, US-guided pericardiocentesis may be performed safely with variable results. Some patients need light sedation (propofol ideally) and a local lidocaine block may be utilized after sterile preparation of the field. Others may not need any sedation at all. The patient is placed in right lateral recumbency with a left sided approach by the sonographer.
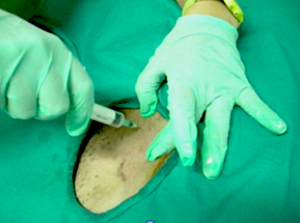
The sonographer stays just above costochondral junction usually IC 4-5 or 5-6 and aim for right auricle without hitting it of course. This is where the tumor (if present) usually starts to bleed into the pericardial sac so aiming there will allow for the most efficient drainage, as it is max volume. The author prefers a 14 to 16g x 2-inch IV catheter flushed with a heparin (diluted in saline) flush, as you would utilize in an IV catheter to avoid clots.
After utilizing the same 2-step sampling approach described earlier (step 1 through the body wall, step 2 through the pericardial sac) and the catheter presence in the pericardial sac can be observed, pull the stylet back a couple of millimeters so only the Teflon is exposed to avoid the stylet from touching the epicardium.
Attach an IV extension set and ideally a suction unit or 60 cc syringe (Have a few handy to trade off).
Large dog tamponade will usually be 200-350 cc. Sometimes the patient may bounce up once they feel better so best to be prepared. Other times the patients is lethargic for a while owing to new systemic volume adjustments. At times the potential cardiac tumors continue to bleed and fill the pericardium as fast as we can remove it.
Don’t give lasix ever in these cases, as they need their minimal internal volume that is fighting against the tamponade. This is not a volume overload disease but a volume contraction disease. Therefore diuresis will make them worse.
Use propofol IV +/- a local lidocaine block at needle site if need be. If a little blood leaks from the pericardium it may assist in an ultrasound guided “fenestration” but of course is not encouraged.
More Ultrasound-Guided Procedures

Bubble Study
The reason to perform a bubble study is to confirm the presence of shunting of blood from venous to arterial flow such as a Reverse VSD or a Reverse PDA.

Gallbladder Motility Study
NPO overnight. Time 0 min: Measure GB in long axis and short axis from subxiphoid approach and right intercostal approach. The proper position is maximum

Intraoperative Ultrasound
We developed this technique to be used on any abdominal organ but is especially effective in case of infiltrative, focal and multifocal GI lesions.

Lindquist Compression Technique For Thoracic FNA
This technique often makes inaccessible thoracic lesions accessible.
Traumatic Catheterization Procedure
Sedation Use largest open-end rigid polypropylene urinary catheter cut diagonally to create a sharp edge like a needle bevel. Lube heavily and pass catheter retrograde
UGELAB for Transitional Cell Carcinoma in the Dog
Dr. Dean Cerf, Ridgewood Veterinary Hospital NJ and Dr. Eric Lindquist, SonoPath.com For More Information Contact Dr. Dean Cerf at Ridgewood Veterinary Hospital, Ridgewood, NJ,

Ultrasound-Guided Lymph Node Culture
This type of lymph node sampling is helpful in determining infected lymph nodes vs. lymphoma. Supplies: 6 cc Luer lock syringe 1cc of saline 2

Ultrasound-Guided Sampling Procedures
Description Ultrasound-guided needle sampling is frequently used in the diagnostic evaluation of patients. Fine needle aspiration has the advantage of requiring minimal or no sedation
