Ultrasound-Guided Sampling Procedures
Home » Resources » Ultrasound-Guided Procedures » Ultrasound-Guided Sampling Procedures

Description
Ultrasound-guided needle sampling is frequently used in the diagnostic evaluation of patients. Fine needle aspiration has the advantage of requiring minimal or no sedation with minimal risk of complications.
However, information obtained may be inconclusive or incomplete and conclusions based solely on cytological specimens may be incorrect. Needle core biopsy samples are generally more accurate than fine needle samples but require some level of anesthesia and have a greater risk of complications depending on the organ system sampled. Regardless, US-guided biopsy is considered a generally safe procedure with minimal risk. Depending on the organ aspirated and the disease processes, the diagnostic yield and accuracy can vary greatly between the procedures. The clinician should be aware of the limitations and benefits of each procedure with the organ and suspected disease process in question.
Diagnostics
Since sampling of either sort may cause some local bleeding, it is important to know the coagulation status of every patient being sampled. A platelet count and clotting panel (OSPT, APTT) should be checked to screen for clotting abnormalities. Increased risk is associated with an elevated clotting time, or with platelet count <50,000.
Clinical evidence of petechiae or ecchymoses should alert the need for a more elaborate coagulation assessment. Our team carries a mobile coagulation analyzer to evaluate OSPT and APTT prior to the sampling procedure. The New Jersey Mobile team follows the following rule for low-risk organ sampling: Biopsy with caution if PT/APTT values that are < 1.3 of normal, FNA if less than 1.5 of normal, treat with vitamin K and recheck if values are higher than that. If the parameters are higher than these standards, the client is informed and a new risk-justification assessment is evaluated. NSAID or aspirin therapy should be discontinued 1 to 2 weeks prior to biopsy, if possible. von Willebrand’s titers and/or buccal mucosal bleeding times should be checked in patients at risk for platelet (functional) abnormalities (including chronic NSAID therapy).
BMBT is the best overall rapid clinical assessment of primary clotting function by means of platelet aggregation. Repeat ultrasound images taken 15 minutes and a few hours after the procedure is the most sensitive means to screen for bleeding complications. A hematocrit should be taken pre- and post -biopsy, although it may take 12-to-24 hours after a bleeding event for it to be reflected in the hematocrit.
Procedures
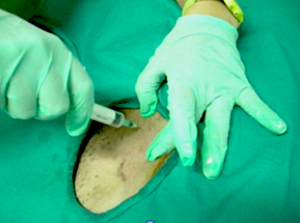
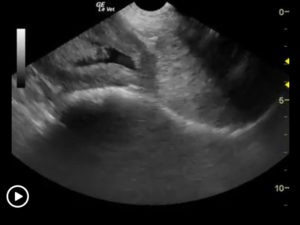
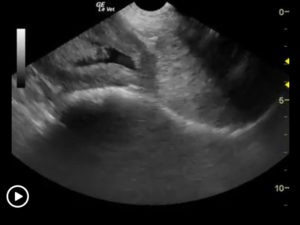
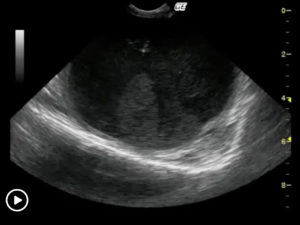
US-guided Fine-Needle Aspiration
Fine needle aspirations, in which a 22-25g needle is used in a “jab” motion, are utilized to retrieve cells from a particular organ system. Sedation is at times necessary with this procedure. Coagulation panels are ideal, but employed at the discretion of the sonographer based on case and sonographic presentation. We are not looking for structural parenchymal changes with this procedure, but simply assessing the cell population present. Mono-population disease (lymphoma, mast cell disease, carcinoma), if present, usually provides at least “suggestive for” if not definitive results by the cytologist. We recommend reading the entire description of the cytology report and not just the “diagnosis” as there is far more information in the description by the cytologist. This holds true for biopsy descriptions provided by the pathologist as well. Assessing the description also allows for evaluation of sample quality. If the sample is of adequate quality, then the results usually lie in the interpretation (a second evaluation may be warranted) or potential biopsy if a largely definitive diagnosis is not achieved and is usually the case if mono-population disease is not evident. If the sample quality is of low yield, then biopsy is likely more appropriate for the underlying pathology in the organ given that some diseased tissue does not readily exfoliate. In an attempt to enhance professional symbiosis between our team and pathologists, we often provide a still image demonstrating the needle position with respect to the pathology being assessed. In this way, there can be little doubt as to what organ was sampled given that the pathologist is only looking at a slide of cells or tissue that can often be poorly reminiscent of the affected organ tissue if afflicted by destructive pathology.
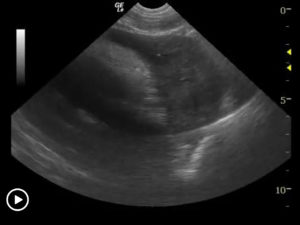
US-Guided Biopsy
In this procedure we are obtaining Tru-cut sections of tissue to evaluate structure of the parenchyma. This is a more definitive procedure regarding mono-population disease (lymphoma, mast cell disease, carcinoma) but is especially necessary when structural evaluation of the parenchyma is necessary for a diagnosis (hepatitis, fibrosing diseases, copper storage disease, protein losing nephropathy, enteropathy with focal lesions, “bridging” lymphoma/IBD to name a few). This procedure absolutely requires a complete coagulation panel as well as sedation (stage 2 or more of anesthesia).
In a large review of post-biopsy bleeding, a decrease of 2% PCV occurred in patients without complications. Dogs with minor complications had a decrease of 8% in hematocrit whereas major complications had a 12% decrease. Cats had an 8% decrease concurrent with both minor and major complications. Patients that are already anemic prior to the sampling procedure require the utmost caution regarding the interpretation of hematocrit alterations. Fluid administration should also be taken into consideration, as intravenous fluids theoretically could dilute clotting factors although no studies have been found to support this theory.
Drainage Procedures
Often we perform drainage procedures for therapeutic and diagnostic value of the pericardium, abdomen, thorax, abdominal abscesses, prostatic abscesses, pancreatic abscesses, infected renal and hepatic cysts, and non-perforating gall bladders. At times, when abscesses have been drained we may inject antibiotic directly back into the abscess cavity given that these regions are often “walled off” from systemic circulation, and therefore not likely to receive systemic antibiotic penetration. Empirically we have seen good results from this procedure but have not published a study on it as of yet.
Conclusion: With careful preparation and patient evaluation, diagnostic samples can be simply and easily obtained with ultrasound, in a relatively non-invasive manner.
References
Roth L: Comparison of liver cytology and biopsy diagnoses in dogs and cats: 56 cases. Vet Clin Pathol 30:35–38, 2001.
Wang KY, Panciera DL, Al-Rukibat RK, et al: Accuracy of ultrasound-guided fine-needle aspiration of the liver and cytologic findings in dogs and cats: 97 cases (1990–2000). J Am Vet Med Assoc 224:75–78, 2004.
Kristensen AT, Klausner JS, Weiss DJ, et al: Liver cytology in cases of canine and feline hepatic disease. Compend Contin Educ Pract Vet 12:1267–1291, 1990.
Willard MD, Weeks BR, Johnson M: Fine-needle aspirate cytology suggesting hepatic lipidosis in four cats with infiltrative hepatic disease. J Feline Med Surg 1:215–220, 1999.
Weiss DJ, Blauvelt M, Aird B: Cytologic evaluation of inflammation in canine liver aspirates. Vet Clin Pathol 30:193–196, 2001.
Center SA, Crawford MA, Guida L, et al: A retrospective study of 77 cats with severe hepatic lipidosis: 1975–1990. J Vet Intern Med 7:349–359, 1993.
Center SA: Diagnostic procedures for evaluation of hepatic disease, in Guilford WG, Center SA, Strombeck DR, et al (eds): Strombeck’s Small Animal Gastroenterology. Philadelphia: Saunders, 1996:130–188.
More Ultrasound-Guided Procedures

Bubble Study
The reason to perform a bubble study is to confirm the presence of shunting of blood from venous to arterial flow such as a Reverse VSD or a Reverse PDA.

Gallbladder Motility Study
NPO overnight. Time 0 min: Measure GB in long axis and short axis from subxiphoid approach and right intercostal approach. The proper position is maximum

Intraoperative Ultrasound
We developed this technique to be used on any abdominal organ but is especially effective in case of infiltrative, focal and multifocal GI lesions.

Lindquist Compression Technique For Thoracic FNA
This technique often makes inaccessible thoracic lesions accessible.
Traumatic Catheterization Procedure
Sedation Use largest open-end rigid polypropylene urinary catheter cut diagonally to create a sharp edge like a needle bevel. Lube heavily and pass catheter retrograde
UGELAB for Transitional Cell Carcinoma in the Dog
Dr. Dean Cerf, Ridgewood Veterinary Hospital NJ and Dr. Eric Lindquist, SonoPath.com For More Information Contact Dr. Dean Cerf at Ridgewood Veterinary Hospital, Ridgewood, NJ,

Ultrasound-Guided Lymph Node Culture
This type of lymph node sampling is helpful in determining infected lymph nodes vs. lymphoma. Supplies: 6 cc Luer lock syringe 1cc of saline 2
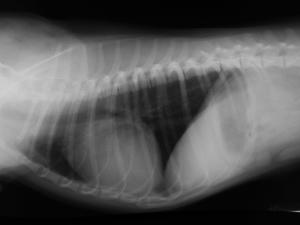
Ultrasound-Guided Pericardiocentesis
History Pericardial effusions typically cause some level of cardiomegaly on radiographs but note poor vascular volume in the pulmonary artery and vein. Muffled heart sounds
