Bubble Study
Home » Resources » Ultrasound-Guided Procedures » Bubble Study
History
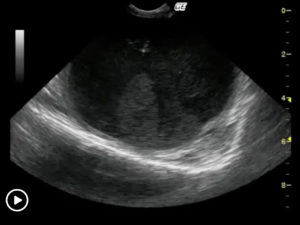
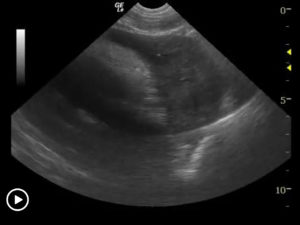
The reason to perform a bubble study is to confirm the presence of shunting of blood from venous to arterial flow such as a Reverse VSD or a Reverse PDA. When severe right sided overload and eccentric hypertrophy is present in patients with exercise intolerance (cyanosis), the clinical sonographer may suspect a reverse VSD or reverse PDA owing to Eisenmenger’s physiology; reversal of flow owing to equalization for right sided compared to left sided pressures.
Procedure
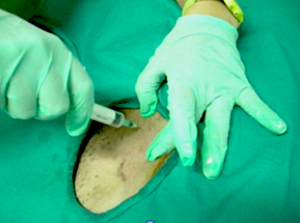
An IV catheter is placed in the cephalic vein. Take 20 cc saline or Hetastarch and draw a few cc of air into the syringe. Agitate the syringe and remove the free air. Dr. Peter Modler demonstrates the materials necessary on the attached PowerPoint “How To Make Bubbles.”
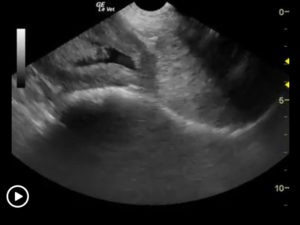
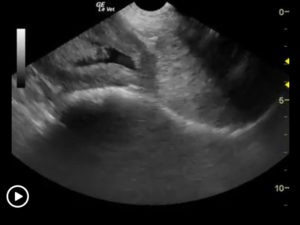
If reverse PDA is suspected then image the abdominal aorta as close to the body wall as possible. Then inject about 10 cc of the agitated saline into the cephalic vein. If a reverse PDA is present then the bubbles will be seen in the abdominal aorta. In a normal patient where a closed venous system is present, the bubbles would dissolve in the pulmonary capillary bed. In the case of reverse VSD, image the heart in 5-chamber right parasternal long axis and concentrate on the region of the interventricular septum where a relatively large defect will usually be present if the patient is starting to reverse the flow from a long standing VSD. If reversal of flow is present then the bubbles will enter the right atrium to right ventricle and cross into the left ventricle and aorta through the defect. The bubbles are then ejected into the aortic circulation without dissolution in the pulmonary circulation.
See this reverse VSD with bubble study performed by Dr. Doug Casey of Vancouver B.C. Canada. English Bay Ultrasound.
More Ultrasound-Guided Procedures


Gallbladder Motility Study
NPO overnight. Time 0 min: Measure GB in long axis and short axis from subxiphoid approach and right intercostal approach. The proper position is maximum

Intraoperative Ultrasound
We developed this technique to be used on any abdominal organ but is especially effective in case of infiltrative, focal and multifocal GI lesions.

Lindquist Compression Technique For Thoracic FNA
This technique often makes inaccessible thoracic lesions accessible.
Traumatic Catheterization Procedure
Sedation Use largest open-end rigid polypropylene urinary catheter cut diagonally to create a sharp edge like a needle bevel. Lube heavily and pass catheter retrograde
UGELAB for Transitional Cell Carcinoma in the Dog
Dr. Dean Cerf, Ridgewood Veterinary Hospital NJ and Dr. Eric Lindquist, SonoPath.com For More Information Contact Dr. Dean Cerf at Ridgewood Veterinary Hospital, Ridgewood, NJ,

Ultrasound-Guided Lymph Node Culture
This type of lymph node sampling is helpful in determining infected lymph nodes vs. lymphoma. Supplies: 6 cc Luer lock syringe 1cc of saline 2
Ultrasound-Guided Pericardiocentesis
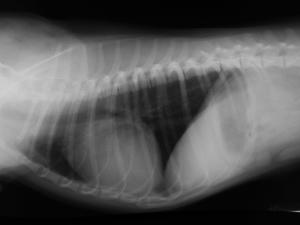
History Pericardial effusions typically cause some level of cardiomegaly on radiographs but note poor vascular volume in the pulmonary artery and vein. Muffled heart sounds

Ultrasound-Guided Sampling Procedures
Description Ultrasound-guided needle sampling is frequently used in the diagnostic evaluation of patients. Fine needle aspiration has the advantage of requiring minimal or no sedation
