
In July 2025, a 9-year-old male neutered Domestic Shorthair cat presented at Stewart’s Mountain View Animal Hospital to Dr. Selena Lusk, with a two-month history of progressive weight loss despite a normal appetite and activity level. The owner reported normal water intake, no vomiting or diarrhea, and two recent episodes of inappropriate urination on the bed. The patient had a known history of cystitis and was maintained on Hill’s Prescription Diet c/d (dry and canned). On physical examination, the cat was bright, alert, and responsive with mild dental tartar and a 2-pound weight loss since February 2025; the remainder of the exam was unremarkable. Dr. Lusk sent out a senior wellness panel and the results are as follows:
CBC: WNL
Chemistry:
- K+ 3.4 (3.7-5.2 mmol/L) LOW
Urinalysis:
- USG 1.011, inactive sediment
Thank you to Dr. Selena Lusk of Stewart’s Mountain View Animal Hospital for her excellent case management and recommendation of additional diagnostic testing to investigate a possible underlying systemic disease. Thanks to Dr. Kathleen Byrnes, SDEP® Clinical Sonographer with Carolina Mobile fueled by SonoPath for her expert imaging, and the proficiency of SonoPath specialist Beth Johnson, DVM, DACVIM, allowing identification of the root cause as a left adrenal mass.
This cooperative approach underscores the value of integrating advanced imaging modalities and specialist consultation into general practice to enhance diagnostic accuracy and patient care options and outcomes.
ULTRASONOGRAPHIC EXAMINATION OF THE ABDOMEN:
Urinary System
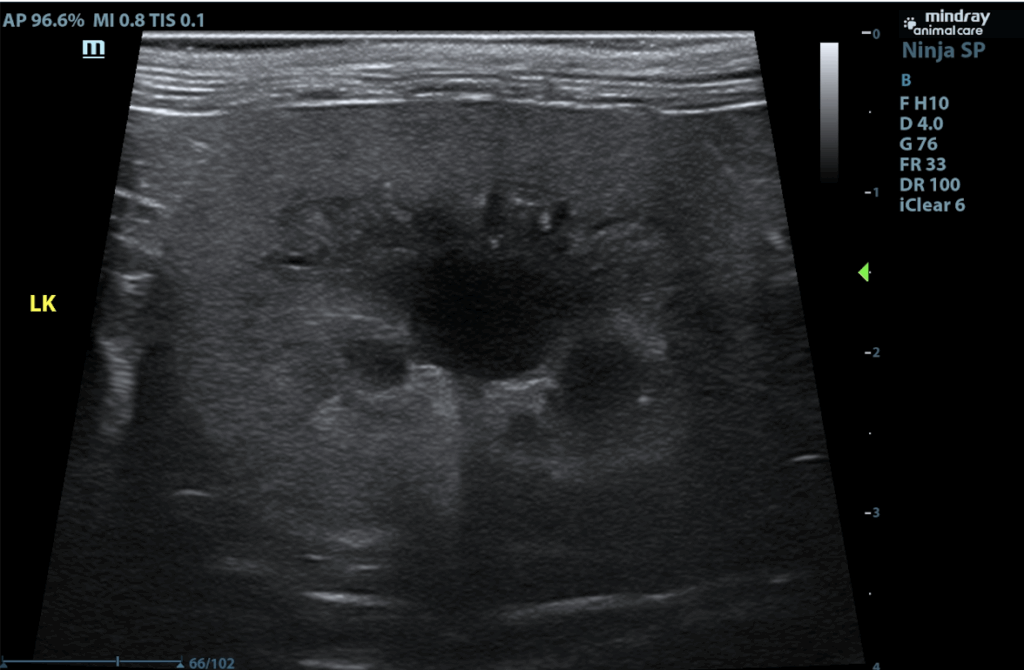
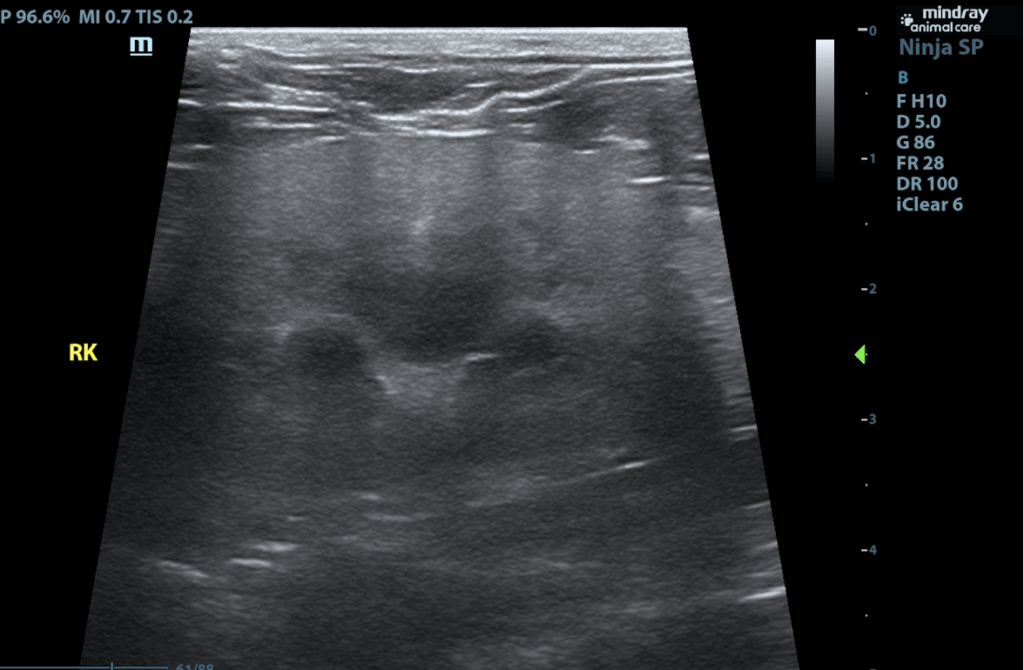
The urinary bladder is adequately distended with anechoic contents. No masses, inflammatory changes, echogenic sediment or cystoliths are observed. The urinary bladder, trigone and visible pelvic urethra are normal in thickness with a smooth mucosal surface. Kidneys are normal in size and contour. A relatively uniform hyperechogenicity is observed with mildly decreased corticomedullary distinction. There is no pyelectasia noted and no mineral is observed. No overt masses/nodules are observed. The left kidney measures 4.19 cm. The right kidney measures 4.33 cm.
Adrenal Glands
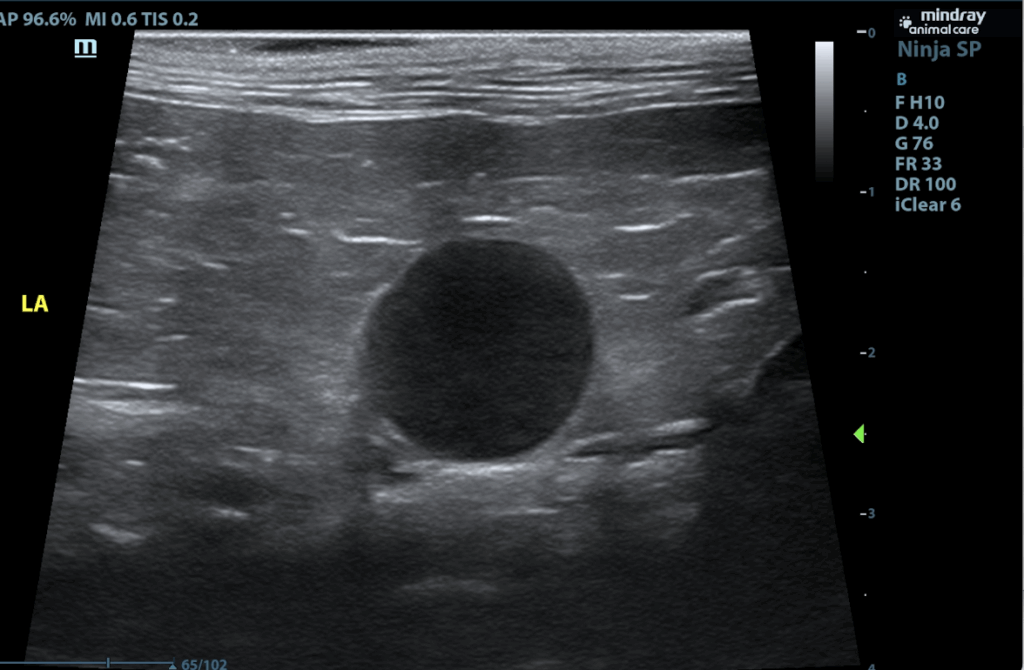
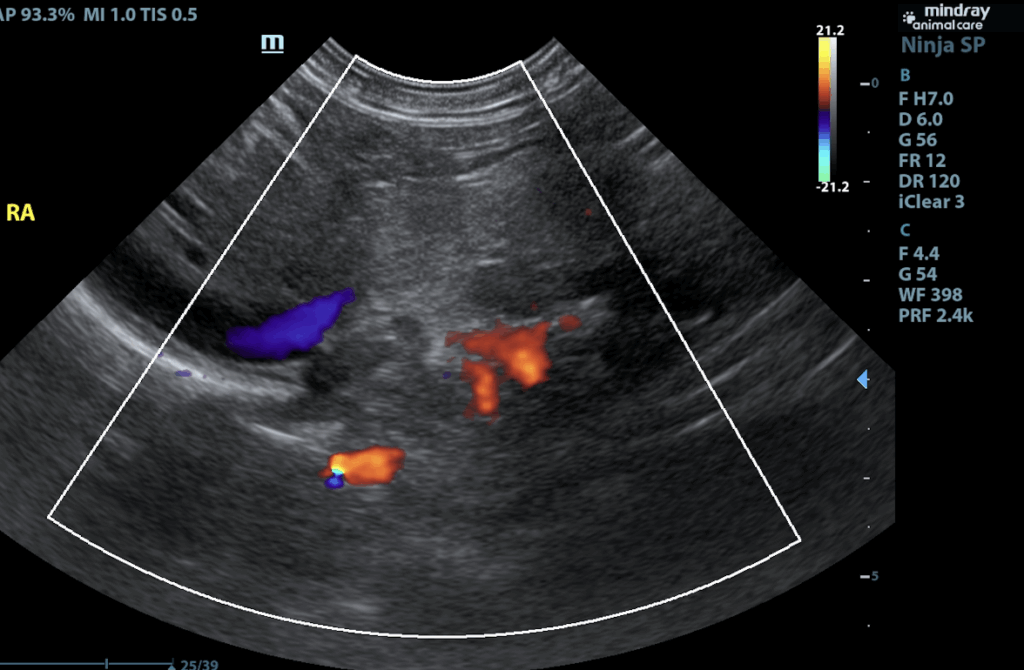
The right adrenal gland is normal in size (0.38 cm at cranial pole and 0.31 cm at caudal pole), shape and overall architecture, echogenicity and echotexture. Visible surrounding vasculature appears normal. The left adrenal gland is enlarged, measuring 1.8 cm long x 1.2 cm thick at the caudal pole, with mild heterogeneous parenchymal changes and an overall egg-shaped hypoechoic appearance, with swollen capsular expansion noted but no evidence of capsular escape or vascular invasion.
Spleen
The spleen is subjectively normal in size with a normal smooth capsular contour. Parenchyma is appropriately finely textured and homogenous with normal echogenicity relative to surrounding tissue (hyperechoic to liver). No focal nodules or masses are observed. Splenic vasculature appears normal.
Liver
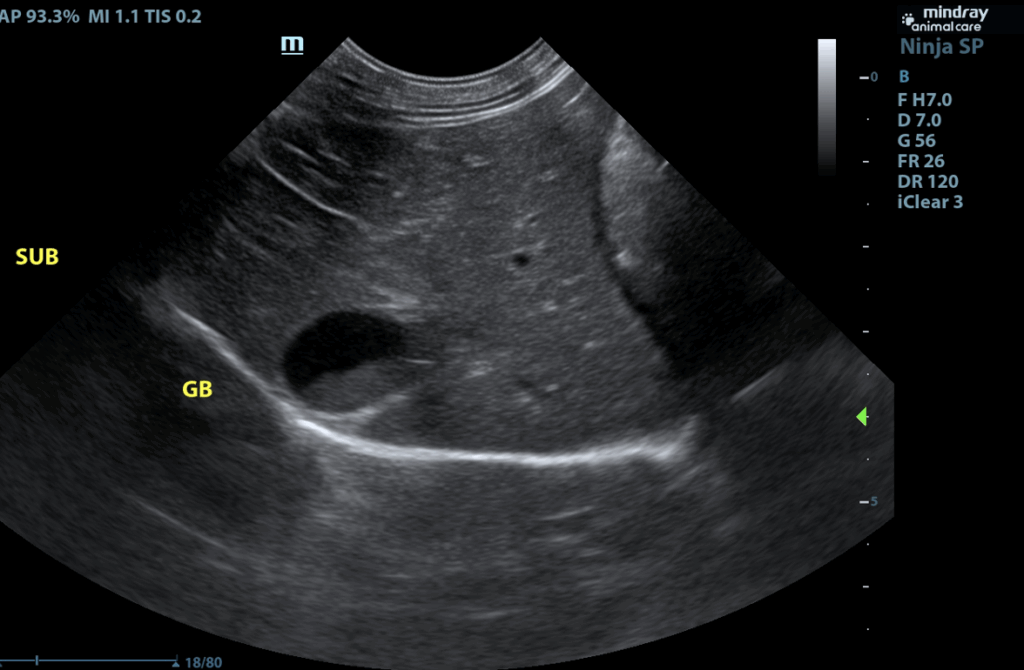
The liver is subjectively normal in size with normal smooth curvilinear peripheral contour. Parenchyma is appropriately hypoechoic to the spleen in echogenicity and appropriately mildly coarse and homogenous in echotexture. No focal lesions are observed. Visible vasculature and biliary tree appear normal without distension or congestion. Gallbladder is moderately distended with anechoic bile as well as suspended and gravity dependent echogenic debris. The wall is smooth without visible thickening. There is no evidence of cystic or CBD dilation. There is no evidence of effusion or inflammation.
Gastrointestinal
The visible stomach wall is normal in thickness and layering. The lumen of the stomach is empty with no evidence of obstruction, foreign material or infiltrative disease. Pyloric outflow tract appears patent. The visible small intestines are normal in wall thickness and layering. Small intestinal motility appears adequate (1-3 contractions per min). The lumen of the small intestine is empty with no evidence of obstruction, foreign material or infiltrative disease.
The visible colon is normal in wall thickness (< 0.2 cm) and layering. Contents are consistent with normal formed feces and gas.
Pancreas
The pancreas that is observed appears appropriately isoechoic to surrounding omental fat. Visible capsule is smooth and normal in contour. Visible pancreatic parenchyma is homogenous and unremarkable. There is no visible pancreatic duct dilation. There is no evidence of active peripancreatic inflammation.
Free Abdomen
There is no visible free peritoneal effusion noted in these images.
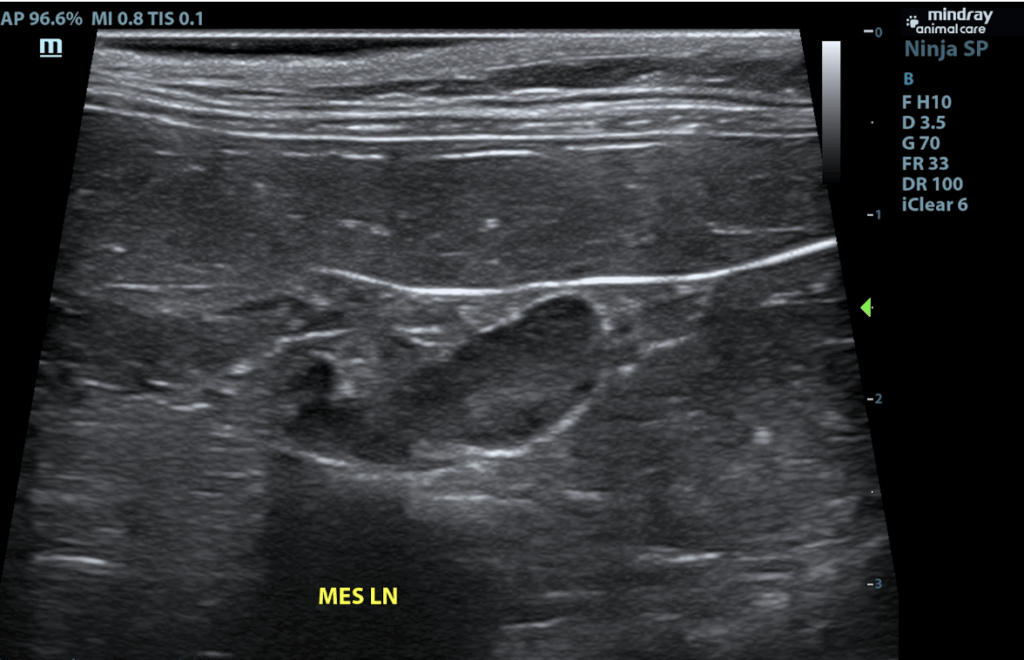
Mesenteric lymph nodes are prominent in size with swollen capsular contour. Normal elongated shape(length to width ratio) is maintained. There is no loss of parenchymal detail.
ULTRASONOGRAPHIC FINDINGS:
- Left adrenal mass.
- Nephritis – This appearance can be consistent with chronic interstitial nephritis or glomerulonephritis. Toxic insult and/or infectious disease (pyelonephritis, FIP in cats, etc.)cannot be ruled out. This finding should be interpreted in combination with suspicion for renal disease and/or supporting laboratory or urinalysis changes.
- Mild gallbladder debris – Cholecystic debris is of unknown clinical significance. It can be seen with biliary stasis from fasting or illness, however, it can also be associated with hepatobiliary disease in cats and should be interpreted in combination with clinical signs such as nausea, inappetence, cranial abdominal discomfort and/or laboratory changes such as increased ALP and/or increased Tbili.
- Very mild reactive mesenteric lymph nodes – infiltrative neoplastic disease cannot be ruled out but is considered less likely.
INTERPRETATION OF THE FINDINGS & FURTHER RECOMMENDATIONS
In a feline patient with hypokalemia, especially with concurrent hypertension, top differential for the adrenal tumor is an aldosterone producing tumor or Conn’s syndrome. Other adrenal disease including hyperadrenocorticism, etc., however, can’t be ruled out, and should be suspected if clinically appropriate and or if hormone testing indicates. Therefore, if not already evaluated, a blood pressure is recommended, as is an aldosterone level +/- cortisol levels. Ultimately, pending workup, a left adrenalectomy may be indicated, but in the meantime, medical management of hypokalemia and hypertension, if indicated, may be appropriate. Spironolactone therapy could be considered.
Further Workup:
- Aldosterone ACTH Stimulation Test
- Aldosterone Baseline 517.3 pg/ml (7.6-261.3
- Aldosterone Post 987.7 pg/ml (38.8-474.5)
Endocrinologist Interpretation: Results indicate increased adrenal activity and aldosterone values are elevated and above the normal reference interval
Blood Pressure:
- Systolic BP 172, 160, 164 mmHg
Diagnosis:
- Left adrenal gland tumor secreting aldosterone causing hyperaldosteronemia, mild hypertension, and hypokalemia
DISCUSSION:
Adrenal tumors are an uncommon finding in cats. They can be functional by producing and secreting a hormone or non-functional. Functional adrenocortical tumors secrete cortisol, progesterone and aldosterone. Functional adrenal medullary tumors are extremely rare and secrete catecholamines(phaeochromocytoma). The most common adrenal tumors in cats are usually cortisol secreting tumors causing Cushing’s Syndrome.
Primary hyperaldosteronism (Conn’s Syndrome) is rare in the cat but may be underdiagnosed. Aldosterone is secreted by the adrenal gland and causes reabsoprtion of sodium and secretion of potassium via the kidneys. Sodium retention causes expansion of extracellular fluid volume. The most common clinical signs seen in cats with hyperaldosteronism are hypertension and muscle weakness due to hypokalemia. Cats can present with non specific signs such as lethargy, inappetance, neck ventroflexion and blindness due to hypertension.
Diagnosis of primary hyperaldosteronism is typically made based on the presence of marked hyperaldosteronaemia, along with hypertension and hypokalemia.
Initial treatment in cats is aimed at correcting hypokalemia, fluid defecits, and acid base imbalances. Potassium gluconate is used as a potassium supplement and spironolactone (an aldosterone receptor antagonist) can be used as well.
Adrenalectomy is the treatment of choice recommended for most cats with unilateral disease that has not metastasized. With successful surgical removal cats can be taken off medication and have survived up to 3 years. The most common complication of adrenalectomy is damage to the caudal vena cava and hemorrhage.
CONCLUSION:
The patient was started on spironolactone and surgery for adrenalectomy was declined. The patient was very difficult to medicate and the owners were unable to continue the spironolactone. Unfortunately, the patient was euthanized approximately 1 month later due to a continued decline in his energy level and weight.
References:
1. Andrew R, Harvey AM, Tasker S. Primary hyperaldosteronism in the cat: A series of 13 cases. J Feline Med Surg 2005;7:173–182.
2. Rose SA, Kyles AE, Labelle P, et al. Adrenalectomy and Caval Thrombectomy in a Cat With Primary Hyperaldosteronism. J Am Anim Hosp Assoc 2007;43:209–214.
3. Rijnberk A, Voorhout G, Kooistra HS, et al. Endocrinology: Hyperaldosteronism in a cat with metastasised adrenocortical tumour. Veterinary Quarterly 2001;23:38–43.
4. Duesberg CA, Nelson RW, Feldman EC, et al. Adrenalectomy for treatment of hyperadrenocorticism in cats: 10 cases (1988-1992). J Am Vet Med Assoc 1995;207:1066–1070.

Looking to enhance the range of your ultrasound diagnostic efficiency?

