A 13-year-old neutered male Chihuahua was presented to Dr. Cox at Countryside Animal Clinic. Due to the patient’s advanced and progressive heart failure, SDEP® Clinical Sonographer Yvonna Aranda from Animal Sounds NW fueled by SonoPath, was promptly called in to perform a thorough abdominal ultrasound. Thanks to the timely interpretation by SonoPath’s Specialist, R. McKenzie Daniel, DVM, DABVP, the veterinary team and family were able to receive clear answers right away.
This case is a strong example of how seamlessly SonoPath collaborates with both the skilled sonographer and the dedicated referring DVM to pursue an accurate diagnosis and guide effective management of a complex condition. Heartfelt thanks to everyone involved in providing such compassionate, life-saving care for this beloved pet!
History:
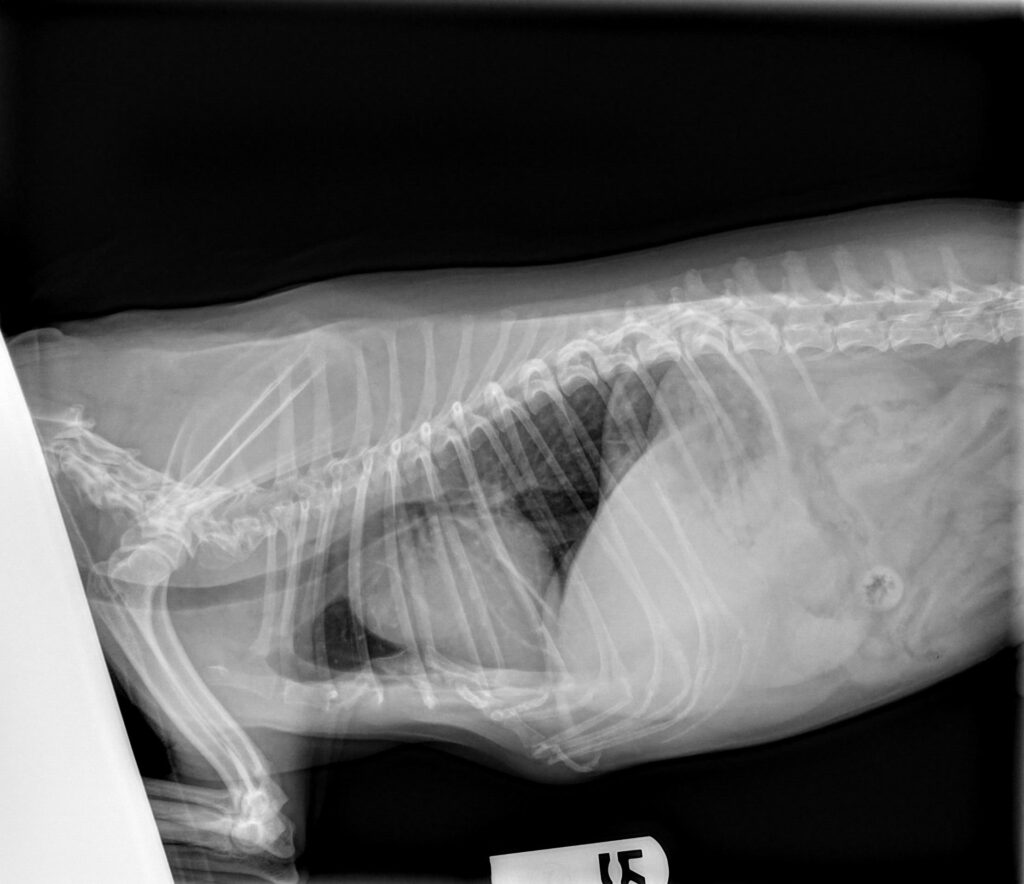
The patient presented for vomiting, labored breathing and a low appetite. The patient has a history of chronic valvular disease (previous echo read by Sonopath). He is currently managed on pimobendan, enalapril and furosemide. Radiographs showed cardiomegaly with possible mild pulmonary edema in the perihilar region.
Bloodwork Results:
CBC:
WBC 19,800 K/uL (4.9-17.6) High
with neutrophilia and lymphopenia
Chem:
ALT 1,020 U/L (18-121) High
AST 103 U/L (16-55) High
ALP 1,778 U/L (5-160) High
TBili 0.5 mg/dL (0-0.3)High
Urinalysis:
USG 1.017, pH 7.5, 1+ protein, inactive sediment
Radiographs taken at the referring veterinary hospital:

Clinical Exam Findings:
On physical exam the patient had a temperature of 104.3 and had mildly increased respiratory effort. He had a heart murmur, increased lung sounds, and became mildly cyanotic with activity.
After bloodwork results were returned an abdominal ultrasound was recommended.
ULTRASONOGRAPHIC EXAMINATION OF THE ABDOMEN:
Urinary System
The urinary bladder, trigone, cystourethral junction, and visible pelvic urethra to a depth of 3 cm exhibited normal thickness and tone. Anechoic urine was present in the lumen with minor non-dependent particulate sediment. The ureteral papillae were normal. The ureters were not visible which is normal. No evidence of inflammatory or neoplastic changes was noted. Normal renal size with asymmetrical margination was present in both kidneys. The renal cortex presented uniformly increased in echogenicity with uniform echotexture. The renal cortex appeared to be hypertrophied resulting in an altered cortex:medulla ratio. Moderate loss of corticomedullary distinction was also present. The renal medullary volume was subjectively reduced. Minor medullary mineral and intermittent small cortical cysts present. The left kidney measured 4.1 cm in length. The right kidney measured 4.6 cm in length.
The area of the aortic trifurcation was free of pathology.
The residual prostate appeared normal and free of pathology
Adrenal Glands
The bilateral adrenal glands were borderline enlarged in size. Mild parenchyma heterogeneity and mild capsule asymmetry was present without suspicion for overt neoplasia. The left adrenal gland measured 2.0 cm length and 0.55 cm width in the caudal pole. The right adrenal gland measured 2.1 cm length and 0.55 cm width in the caudal pole.
Spleen
The spleen exhibited primarily finely textured and homogenous parenchyma which was hyperechoic to the liver and renal cortical parenchyma. Solitary to intermittent, well-defined, symmetrical, hyperechoic nodules were present throughout the medial parenchyma. An example measured 0.37 cm in diameter. The capsule was smooth and regular without apparent expansion. The splenic vasculature at the hilus was normal in volume with no evidence of congestion or thrombosis. Acute to chronic inflammatory or neoplastic changes were not noted. The hyperechoic nodules tend to trend benign and are most consistent with benign hyperplasia or myelolipomas.
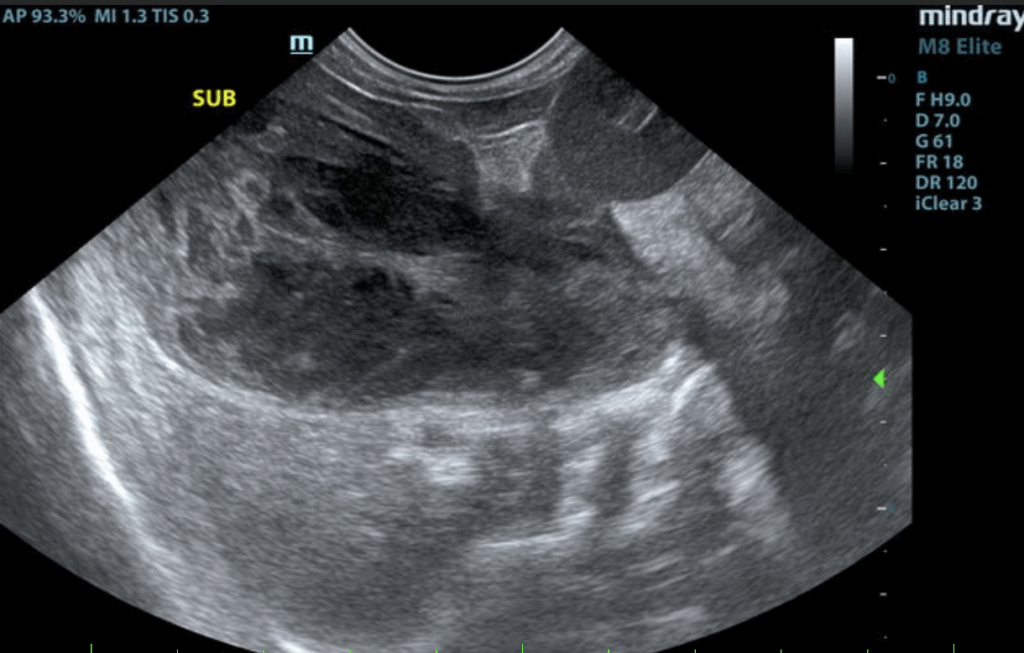
Liver/Gallbladder
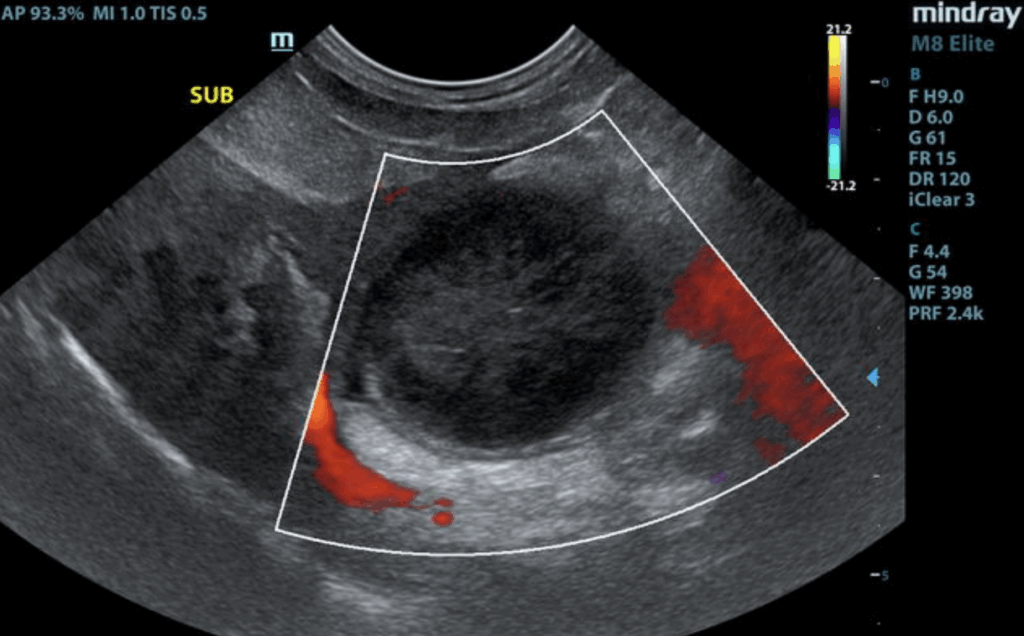
The liver presented enlarged in size. The parenchyma of the liver was subjectively normal in echogenicity compared to the spleen and renal cortices. The liver parenchyma was uniform with a mildly coarse echotexture. The capsule of the liver was symmetrically rounded to mildly swollen in margination. A solitary, small ventrocaudal thinly walled intraparenchymal cyst was present. The hepatic and portal vasculature were normal in appearance without signs of congestion. The gallbladder was distended in size with echogenic thickening of the gallbladder wall. There was biliary sludge that appeared to be non-mobile and organized. A stellate pattern to the organized biliary sludge was present. Regional pericholecystic omental inflammation without overt effusion was present. The common bile duct was not visualized.
Gastrointestinal
The stomach presented wall thickening secondary to echogenic mucosa hypertrophy. Intact wall layering was maintained and distinct. Mild gastric distension with primarily anechoic fluid and chyme was present. No evidence of shadowing gastric echo, overt foreign material or mechanical pyloric outflow obstruction. The small intestine presented intact wall layering with 1:3 muscularis/mucosa ratio. Subtle segmental hyperechoic intestinal mucosal speckling present with minor ileus. The lumen of the small intestine was empty with no signs of obstruction or foreign material.
Normal visible colon wall layers were present with apparent formed feces in lumen.
Pancreas
The right pancreas was normal in size and contour with isoechoic to heterogeneous parenchyma compared to adjacent omentum. No signs of active inflammation or neoplasia.
Free Abdomen
No omental masses, overt lymphadenopathy or peritoneal effusion was present.
ULTRASONOGRAPHIC FINDINGS:
Primary
• Gallbladder mucocele with peripheral inflammation.
• Hepatopathy-subjective acute on chronic.
• Gastroenteritis pattern.
• Pancreatic remodeling.
• Borderline bilateral adrenomegaly.
Secondary
• Benign splenic nodules consistent with myelolipomas.
• Chronic renal changes exhibiting minor medullary mineral and cortical cysts.
INTERPRETATION OF THE FINDINGS & FURTHER RECOMMENDATIONS:
Given gallbladder mucocele with pericholecystic inflammation and concurrent hepatopathy, cholecystectomy with hepatic biopsies assuming normal clotting status is warranted. However, given clinical history in this patient, surgical considerations may be limited. Likewise, even with surgery, overall prognosis is considered guarded given the possibility of mild bile leakage or possible emerging bile peritonitis. Gallbladder mucocele may be associated with Cushing’s syndrome or hypothyroidism. Hepato-gastrointestinal support would be reasonable. If surgery is elected in this patient, recheck echocardiogram indicated to assess anesthetic risk.
Discussion:
A gallbladder mucocele develops due to an abnormal buildup of inspissated or thickened bile and/or mucous in the gallbladder lumen. The gallbladder and biliary tree may become distended with this gelatinous material and cause signs of extrahepatic biliary obstruction(EHBO). When distended, the gallbladder wall becomes necrotic, can rupture and result in bile peritonitis. The exact cause for development of a gallbladder mucocele is unknown but affected dogs have hyperlipidemia and concurrent endocrinopathies such as Cushing’s, hypothyroidism, pancreatitis or diabetes mellitus. A breed predisposition may also exist in the Shetland Sheepdog, Border Terrier, Miniature Schnauzer, and Beagle. It is common in older small to medium breed dogs and rarely seen in the cat.
Affected patients typically present with nonspecific signs such as lethargy, vomiting, diarrhea, abdominal pain, inappetence, polyuria/polydipsia and icterus. Bloodwork can show a leukocytosis with degenerative neutrophilia, elevated ALKP, ALT, AST, GGT, cholesterol, and total bilirubin. Amylase and lipase can also be elevated.
Abdominal ultrasound is diagnostic for a gallbladder mucocele. A gallbladder mucocele typically has a striated, stellate appearance and the material is not mobile. Common findings on ultrasound include a thickened gallbladder wall, free fluid and increased echogenicity of surrounding tissue in the gallbladder fossa. Gallbladder rupture is diagnosed on ultrasound by a discontinuity of the gallbladder wall, hyperechogenicity of the cranial abdominal fat, free peritoneal fluid, or a free, well-organised mucocoele within the peritoneal cavity.
Asymptomatic cases can be managed medically with ursodiol, hepatic protectants, and frequent monitoring as these cases can develop into an emergency very quickly. Surgery is the treatment of choice. There is a 66% survival rate associated with cholecystectomy. Factors associated with in hospital death were increased age, hypotension during surgery, and gallbladder rupture. 1 2 3


Patient Outcome:
The patient presented for cholecystectomy on 4/24/25. On exploratory the gallbladder was very firm and distended with thinning serosa. It was adhered to the liver and parts of the omentum were adhered to the gallbladder wall. The cystic duct was ligated and the common bile duct was evaluated for patency. The surgery went well and the patient was discharged. The following day the patient was doing very well and “eating a lot” according to the owner. Bloodwork was repeated approximately 2 weeks later and showed significant improvement.
Repeat Bloodwork
5/8/25
ALT 137 U/L (18-121) High (Previous 1,020 UL)
AST 23 U/L (16-55) Normal
ALP 603 U/L (5-160) High (Previous 1,778 U/L)
TBili 0.1 mg/dL (0-0.3) Normal
References
1. Jaffey JA, Kreisler R, Shumway K, et al. Ultrasonographic patterns, clinical findings, and prognostic variables in dogs from Asia with gallbladder mucocele. Journal of Veterinary Internal Medicine 2022;36:565–575.
2. Smalle TM, Cahalane AK, Köster LS. Gallbladder mucocoele: A review. J S Afr Vet Assoc 2015;86:1318.
3. Jaffey J a., Graham A, VanEerde E, et al. Gallbladder Mucocele: Variables Associated with Outcome and the Utility of Ultrasonography to Identify Gallbladder Rupture in 219 Dogs (2007–2016). Journal of Veterinary Internal Medicine 2018;32:195–200.

Looking to enhance the range of your ultrasound diagnostic efficiency?

