Severe Mitral Valve Stenosis In A 5-Year-Old MN Bull Terrier. Our Case Of the Month December 2023

Teamwork definitely makes the dream work! We would like to give credit to some of the many doctors at Newton Veterinary Hospital who managed this challenging cardiac case for their patient, a 5-year-old MN Bull Terrier. Dr. Amira Guerrero, Dr Emily Barron, Dr. Hannah Kim, and Dr. Elizabeth Chabora, as well as all of the hardworking team members at NVH, provided compassionate care for this sweet dog with an unfortunately declining heart condition. Diane McFadden, BS, RVT, SDEP® Certified Clinical Sonographer and Director of Education captured the hind-end diagnostic images for this case with interpretation and medical recommendations provided by Maggie Machen Lamy, DVM, DACVIM (Cardiology)
History
The patient, with a history of cardiomegaly, left atrial enlargement, and CHF, presented for coughing. The patient was admitted to the hospital for treatments and further diagnostics. Medications given: furosemide 65mg IV initially Q4h, then Q8h, Cerenia 22mg Q24h, Unasyn 660mg Q8h, pimobendan 5mg Q12h (just started once hospitalized), metronidazole 250mg Q12h, and pantoprazole 22mg Q24h. Abnormal CBC results: Neutrophils 224.
Ultrasound Findings
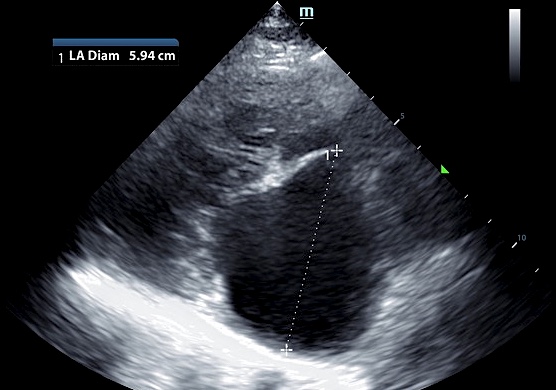
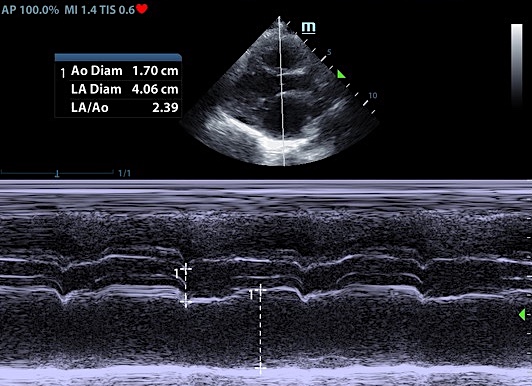
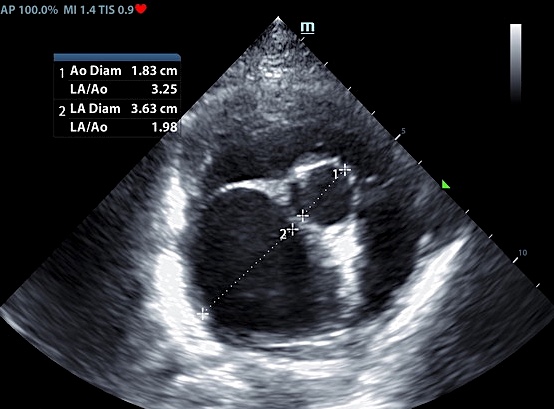
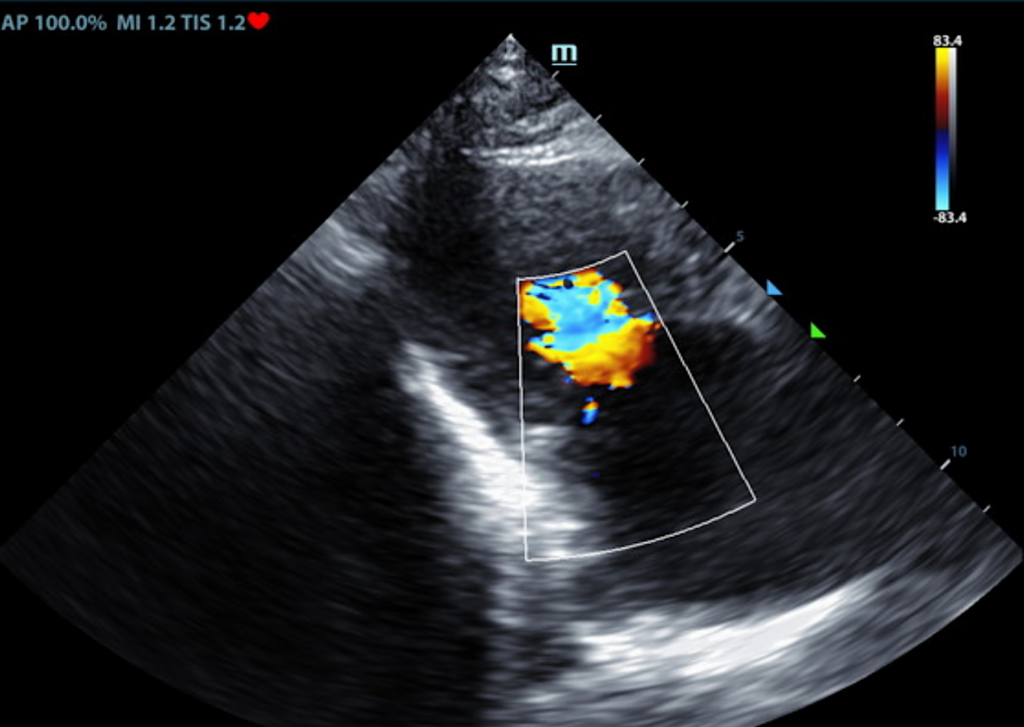
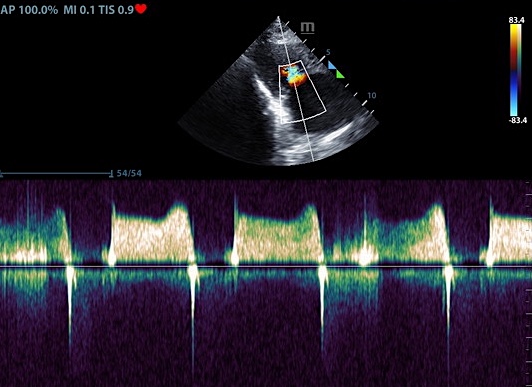
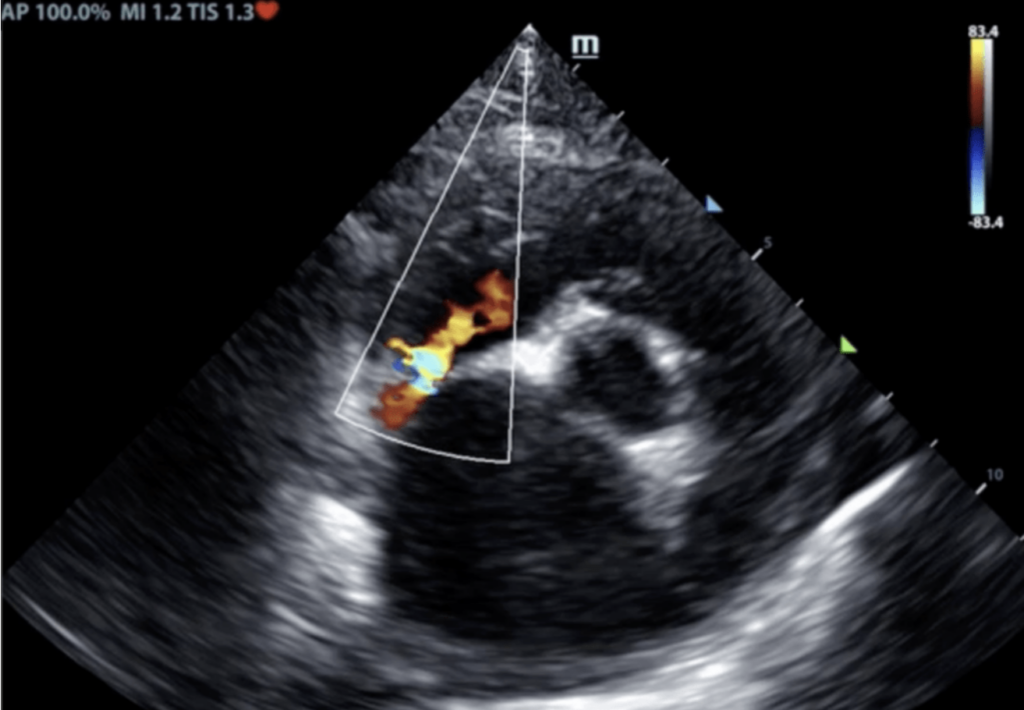
The left atrium was markedly dilated and bulbous in appearance. Flow was suspected to be crossing the interatrial septum (L-R) most consistent with a patent foramen ovale (PFO). The mitral valve was thickened with an elongated club-like anterior leaflet. Lack of excursion in diastole was consistent with significant stenosis. Mitral inflows supported a stenotic pattern. Mild central mitral regurgitation was present with a normal velocity. Trace tricuspid regurgitation was seen.
Diagnosis
Severe mitral valve stenosis, with CHF the likely cause of the current clinical signs.
Interpretation of the Findings
The primary abnormality identified is severe mitral valve stenosis. This is a form of mitral valve dysplasia where the valve does not open adequately leading to marked left atrial pressure elevation. There is also a mild mitral regurgitation, which is commonly seen with this disorder. It is common for mitral stenosis to remain silent as a diastolic murmur is often not appreciated on exam and is only diagnosed once decompensation develops, as is suspected to be the case here. Finally, flow is suspected to be crossing the atrial septum from the LA to the RA. There is no obvious defect appreciated, likely suggesting a patent foramen ovale is present. This is benign, and likely helps relieve some degree of LA pressure. No additional issues are identified.
“tilted brick” position.
the mitral valve.
Patient information
- 5 years old
- Male neutered
- Bull Terrier
Further Recommendations
An advanced interventional procedure may be available at select universities to help relieve left atrial pressure elevation with mitral stenosis. Consultation with an academic facility was strongly recommended. Prognosis is poor in this case, with high risk for complications such as recurrent congestive heart failure, malignant arrhythmias and sudden death. Medications and close monitoring will help give the best prognosis possible; however, the average survival time with this condition is less than 6 months. Monitoring at home for cough, lethargy, inappetence, collapse/fainting episodes or increase in respiratory rate or effort is encouraged. Monitoring of sleeping breathing rates is recommended to screen for recurrent CHF at home. Moderate activity restriction is advised. Omega fatty acid supplementation and mild salt restriction may be of some long-term benefit. Continue hospitalization until stable with injectable Lasix and oral pimobendan therapy. Discharge on the following: administer pimobendan 0.3mg/kg PO q12h. Administer furosemide 1-2mg/kg PO q12h. Institute spironolactone 1-2mg/kg PO q12h. Consider referral as discussed once stable. Recheck renal panel and blood pressure in 10-14 days to ensure tolerance of medications, then every 3-4 months lifelong. A recheck echocardiogram is recommended in 6 months to screen for progression.
Current Case Status
The patient presented 3 months later for coughing. On physical exam the patient was tachycardic, had an increased respiratory rate and effort with crackling in all lung fields, and a distended abdomen. Radiographs showed pleural effusion and an enlarged right atrium. Options were discussed: referral to a cardiologist, change/increase in meds, as well as quality of life and humane euthanasia. The owners elected to continue medications with an increase in dosing. Pimobendan 7mg BID, Lasix 20mg x 3 tabs TID to possibly 4 tabs TID if no improvement is seen, and spirinolactone 25mg x 1 tab BID. At last follow up, the patient was found to be doing ok on current treatments.
SDEP® Echo Ultrasound Education and Training
If you are interested in learning how to perform echocardiograms utilizing SonoPath’s SDEP® protocol, join us via our virtual option at our next SDEP® Echo ultrasound training lab, March, 22-24, 2024 or in-person at our SDEP® Echo hands-on ultrasound lab, September, 13-15, 2024.
