VSD, CHF, and Thoracic Mass In A 4-Year-Old Intact Male Sphynx Cat: Our Case Of the Month February 2023

Echocardiograms are vital for the diagnosis and management of cardiac disease. Changes in the heart can develop slowly, or in the case of this patient, who has a ventricular septal defect (VSD), can progress more rapidly. The patient was diagnosed with VSD at his initial ultrasound. Within 4 months, the patient had gone into congestive heart failure with a moderate amount of pleural effusion present. 8 months from the initial ultrasound, the patient was dealing with a large amount of pleural effusion and a large thoracic mass was discovered. Serial ultrasounds performed by Kelly Vazquez, CVT, SDEP® certified clinical sonographer for SonoPath Mobile Veterinary Ultrasound; specialist interpretations by Eric Lindquist, DMV, DABVP, Cert. IVUSS, Maggie Machen, DVM, DACVIM (Cardiology) and R. McKenzie Daniel, DVM, DABVP.
Image Interpretation
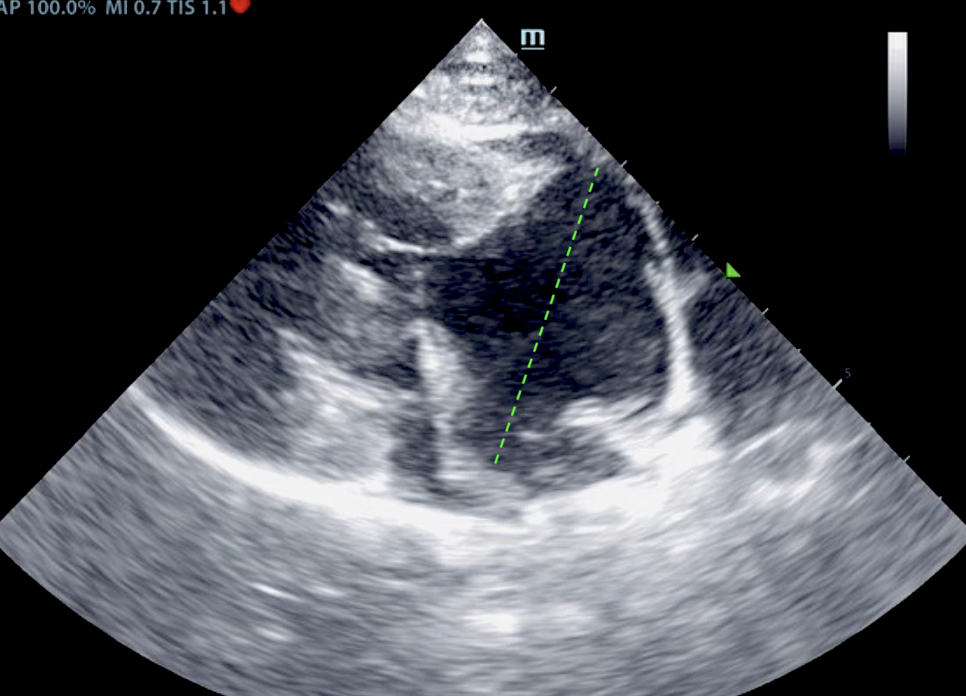
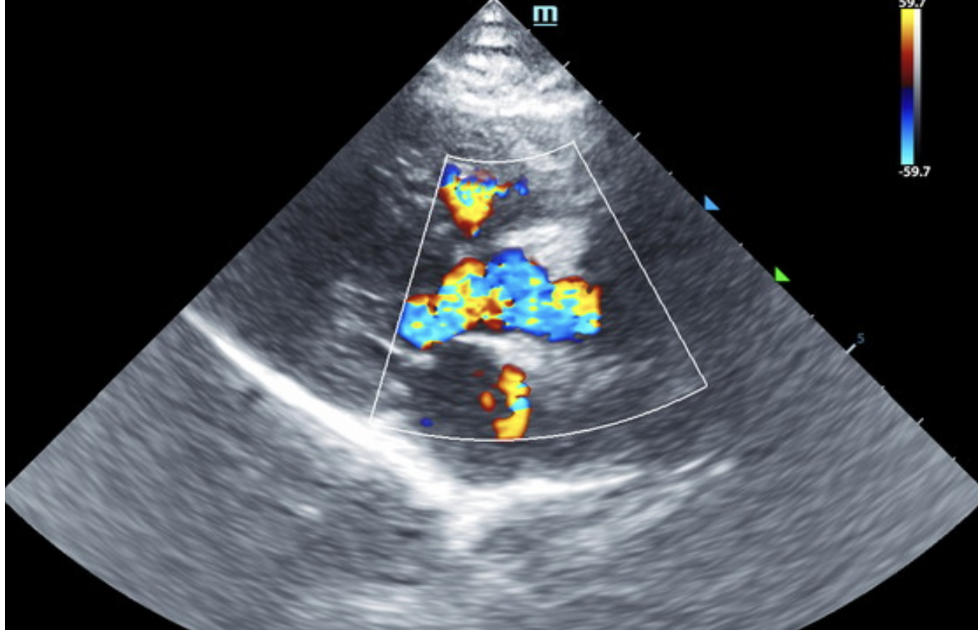
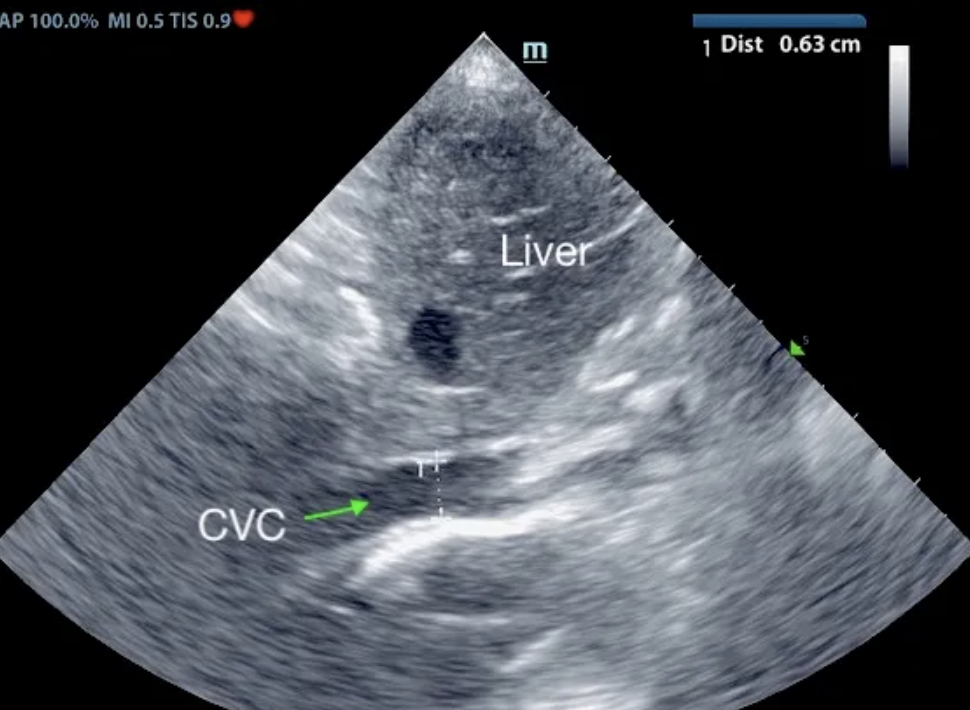
Initial echo: The right atrium was severely enlarged in this patient, measuring 3.0 cm in width. The left atrial size was normal to subnormal at 0.8 cm. The left atrial and left ventricular volumes were normal to subnormal with a large ventricular septal defect noted at the membranous septum, causing volume overload in the right heart. Trivial mitral insufficiency noted yet not clinically significant. Secondary tricuspid insufficiency noted with severe right atrial enlargement. The bi-directional flow noted in the ventricular septal defect is indicative of Eisenmanger’s physiology or reversal of flow, owing to equivalent pressures in the right and left heart. Right ventricular hypertrophy noted. Mild increased pulmonic outflow velocity noted, considered compensatory. No pericardial or pleural effusion noted.
Patient Information
Age:
Gender:
Species:
4 Years
Male, intact
Feline
History
- Heart Murmur
- Lethargy
- Respiratory distress
Clinical Signs
- Ascites
- Heart Murmur
- Lethargy
- Pleural effusion
- Respiratory distress
Exam Findings
- Ascites
- Heart Murmur
- Respiratory Distress
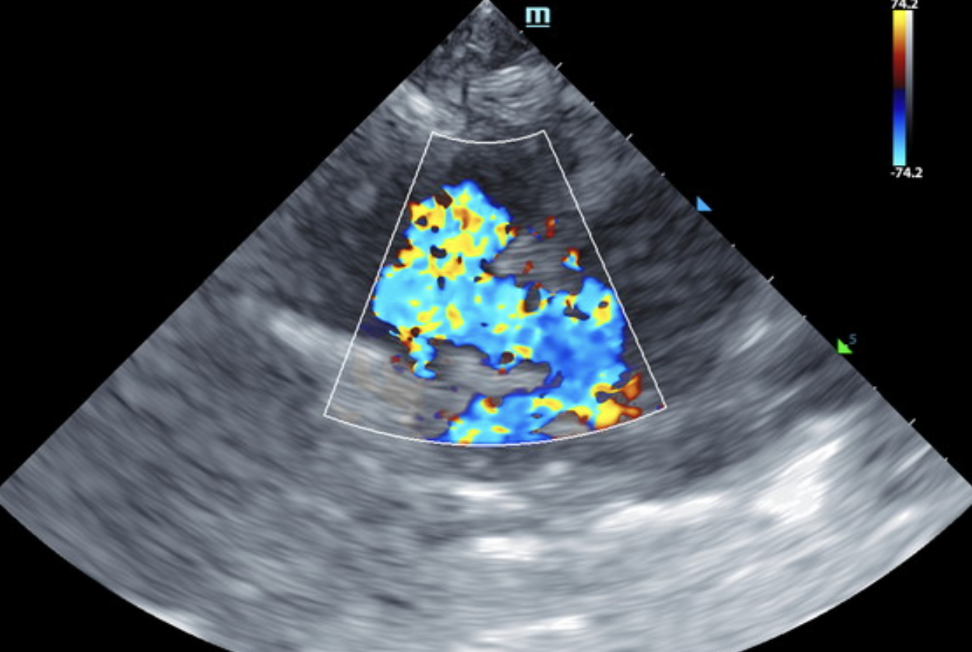
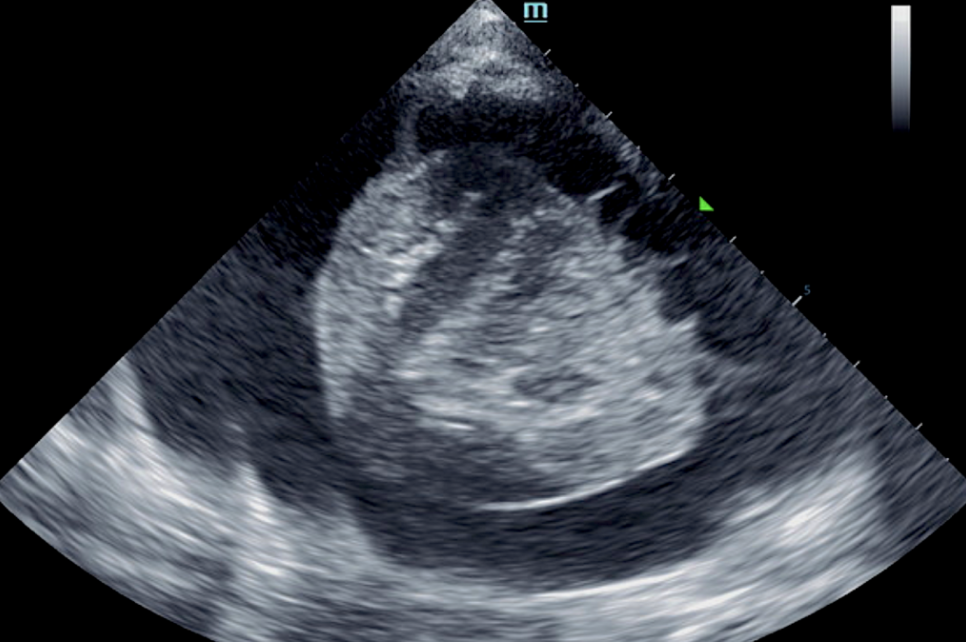
At 4-month recheck echo: The left atrium is normal to slightly volume underloaded. The right atrium is markedly enlarged; no obvious smoke. The right ventricle is mildly enlarged with mild RV hypertrophy; however, the systolic function is subjectively intact. Mild central tricuspid regurgitation. Flow through the RVOT is borderline elevated. A VSD is unable to be visualized on 2D imaging. An abnormal jet is seen entering the mid-RV however, consistent with this previous diagnosis. Trivial pericardial effusion. Moderate volume pleural effusion and ascites is seen with hepatic congestion. No obvious cardiac tumors.
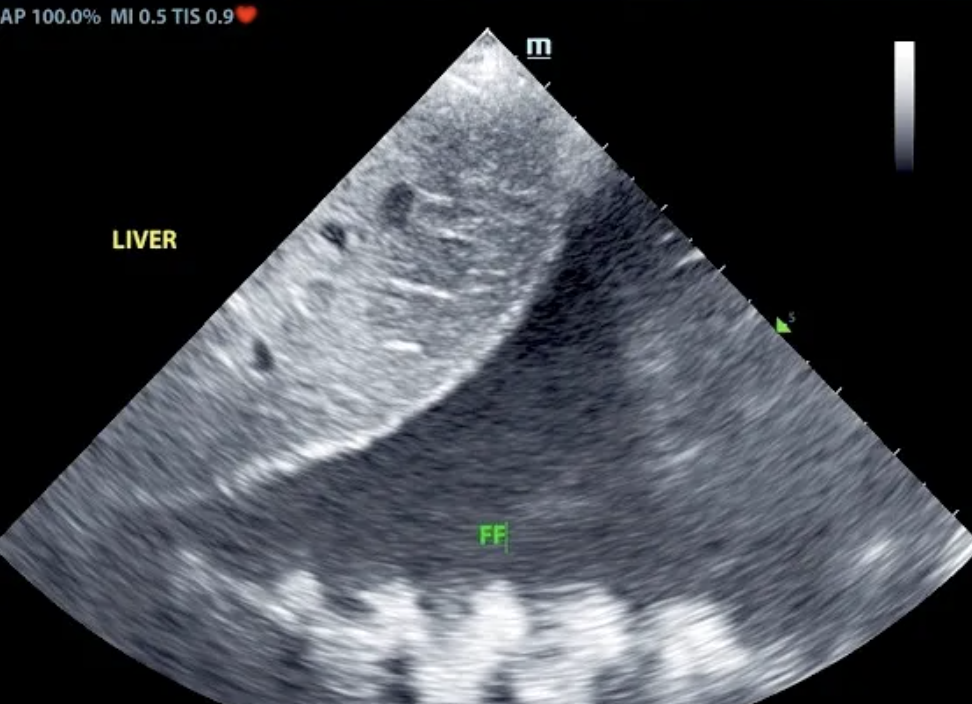
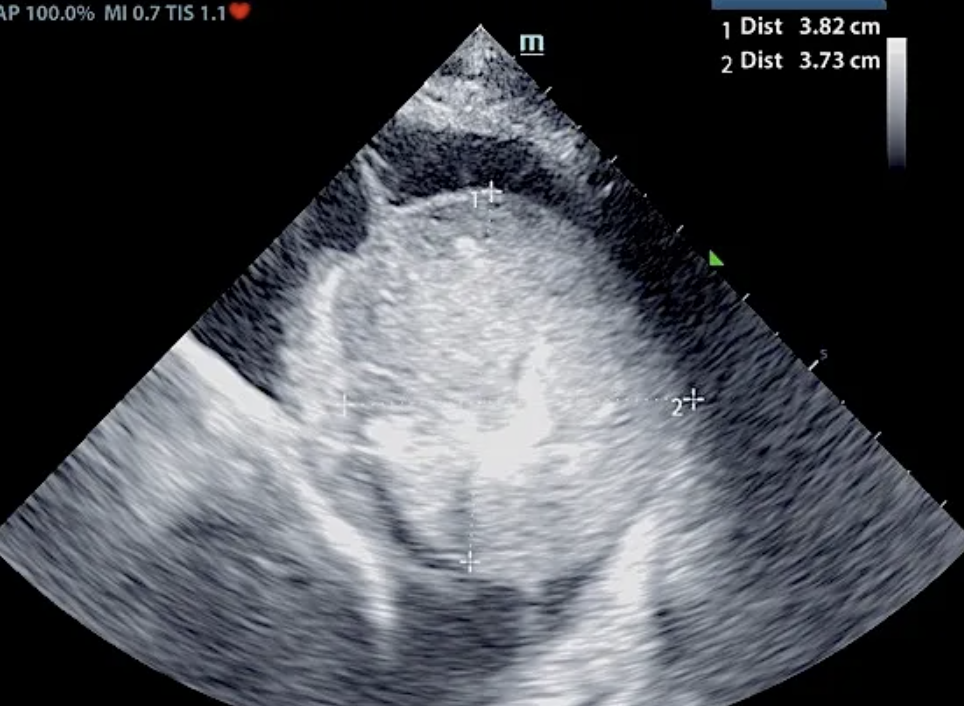
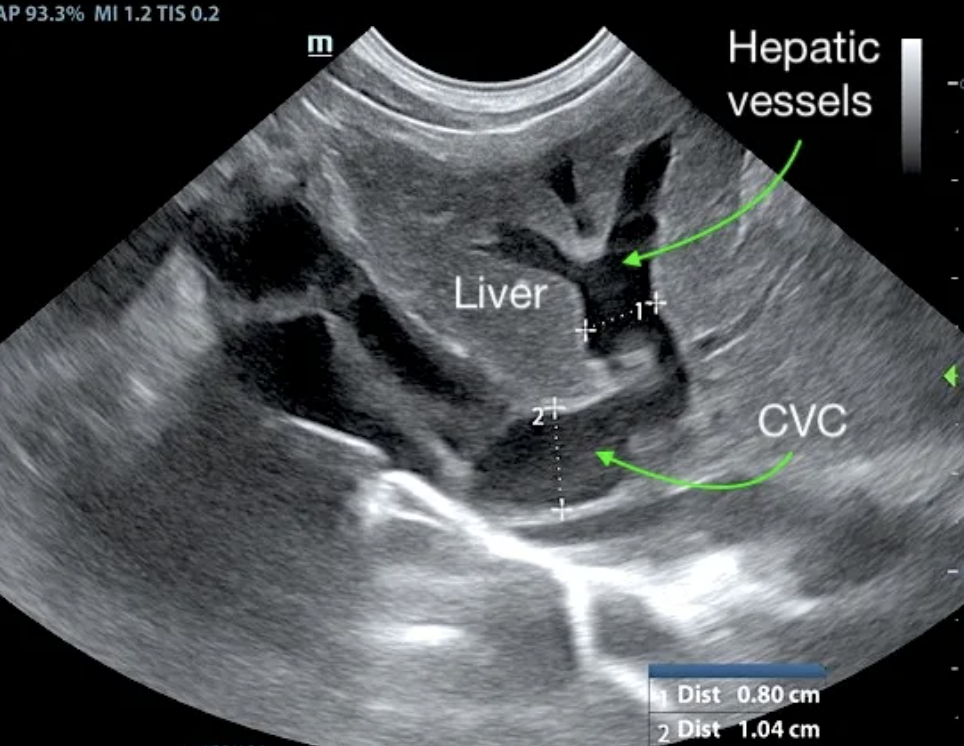
At follow up echo 8 months from initial ultrasound: Subjective mild reduced LV volume is present. Marked right atrial enlargement (measuring 3.6 cm diameter) with concurrent right ventricular enlargement exhibiting potential evidence of mild right ventricle concentric hypertrophy was noted. Moderate volume pleural effusion was present. An unspecified spherical non-homogeneous mass lesion was noted adjacent to the heart measuring approximately 3.7 cm in diameter. Brief sonographic assessment of the liver revealed subjective caudal vena cava and hepatic vein dilation suggestive of emerging congestive criteria.
These findings are compatible with an extensive infiltrative process with differentials including hepatocutaneous syndrome, neoplasia such as hepatocellular carcinoma, extensive nodular hyperplasia or fibrosis associated with a chronic inflammatory process. Cirrhosis is considered less likely, given the suspected normal to increased volume of the liver.
None as clinical and sonographic presentations evaluated by the dermatologist consistent with hepatocutaneous syndrome. Owner did not permit sampling of the liver.
DX
Ventricular septal defect • Eisenmenger’s physiology • Right sided volume overload • Pleural effusion • Hepatic congestion • Thoracic mass
Outcome
Initial echo: Concern for right sided heart failure. Prognosis long term is poor. This is a congenital lesion with secondary emerging right sided heart failure. At 4-month recheck: The cause of bi-cavitary effusion is right-sided cardiomyopathy. There are severe right heart compensatory changes, which would suggest elevated risk for decompensation. Immediate hospitalization and lifelong cardiac support is recommended. Thoracocentesis and/or abdominocentesis should be considered to improve patient stability. At follow up echo 8 months later: Complex case with significant right cardiomyopathy. Given the age of the patient and this presentation, potential considerations may include stenotic disease, tricuspid dysplasia, non-obvious pulmonary hypertension, or other congenital vs. acquired defect. The pleural effusion may be multi-factorial in origin given the concurrent unspecified pericardial to thoracic mass lesion, although given evidence of early hepatic congestive criteria, the patient is likely technically in right heart failure. A very guarded to potentially unfavorable prognosis is likely indicated. At the time of this article, the owners were keeping the patient as comfortable as possible with thoracocentesis to aspirate the pleural effusion, making breathing easier and buying this sweet, velvety fellow a bit more time.
Comments
Ventricular septal defects (VSDs) are most commonly located in the perimembranous portion of the septum, high in the ventricular septum immediately beneath the right and noncoronary aortic valve cusps on the left and just below the cranioseptal tricuspid valve commissure on the right. They vary in size and hemodynamic significance. Doubly committed juxta-arterial septal defects (located beneath the aortic valve on the left and beneath the pulmonic valve on the right) and muscular septal defects (located at any site along the muscular septum) may also be seen. Ventricular septal defects may be seen with other congenital cardiac anomalies. Credit: MSD Manual LINK
Congestive heart failure (CHF): Left-sided congestive heart failure occurs when the pressure inside the blood vessels in the lungs increases causing fluid to seep from the vessels into the surrounding lung tissue. Right-sided congestive heart failure is similar to left, but causes pleural effusion and/or abdominal ascites. Credit: MSD Manual: LINK.
Eisenmenger’s physiology describes changes that occur when a left to right shunting cardiac defect, eg VSD, PDA, causes pulmonary overperfusion, leading to pulmonary hypertension and eventually reversed shunting (right to left) as the right heart pressures increase and become equal to or greater than systemic arterial pressures. Credit: Vetlexicon™ LINK.