In August 2025, a 7-month-old male intact Golden Retriever presented for workup of a possible liver shunt. During his puppy vaccine visits, he appeared clinically healthy aside from being mildly underweight. At approximately 5 months of age, he developed a decreased appetite, polyuria, and polydipsia. The owner reported offering several different diets, noting that he has never been a “good eater”.
On physical examination, the patient was bright, alert, and responsive, and the remainder of the examination was unremarkable. A sick panel was submitted, and abdominal ultrasound and bile acids testing were recommended. Special thanks to Dr. Bott-Wentworth from Willowbrook Animal Clinic, for her care and case management, and to SDEP® Certified Sonographer Kerri Becker for performing an excellent ultrasound, which allowed Dr. Eric Lindquist to provide a thorough interpretation and ultimately obtain the answers this patient needed. The results are as follows:
CBC:
- HCT 38.4 (41-60%) LOW
- HGB 12.5 (14.6-21.7g/dL) LOW
- Monocyte 1060 (145-736 /ul) HIGH
- Eosinophil 57 (141-1927 /uL) LOW
Chemistry:
- Creatinine 0.3 (0.5-1.5mg/dL) LOW
- Phosphorus 7.0 (2.5-6.1 mg/dL) HIGH
- Total Protein 5.0 (5.5-7.5 g/dL) LOW
- Albumin 2.6 (2.7-3.9 g/dL) LOW
- ALKP 262 (5-160 U/L) HIGH
- ALT 163 (18-121 U/L) HIGH
- AST 138 (16-55 U/L)HIGH
- Amylase 305 (337-1469 U/L) LOW
Urinalysis:
- USG 1.015 , 3+ Ammonium Mg Phosphate crystals
Bile Acids:
- Pre: 1.6 (0-14.9 umol/L)
- Post: 28 (0-29.9 umol/L)
ULTRASONOGRAPHIC EXAMINATION OF THE ABDOMEN:
Urinary System:
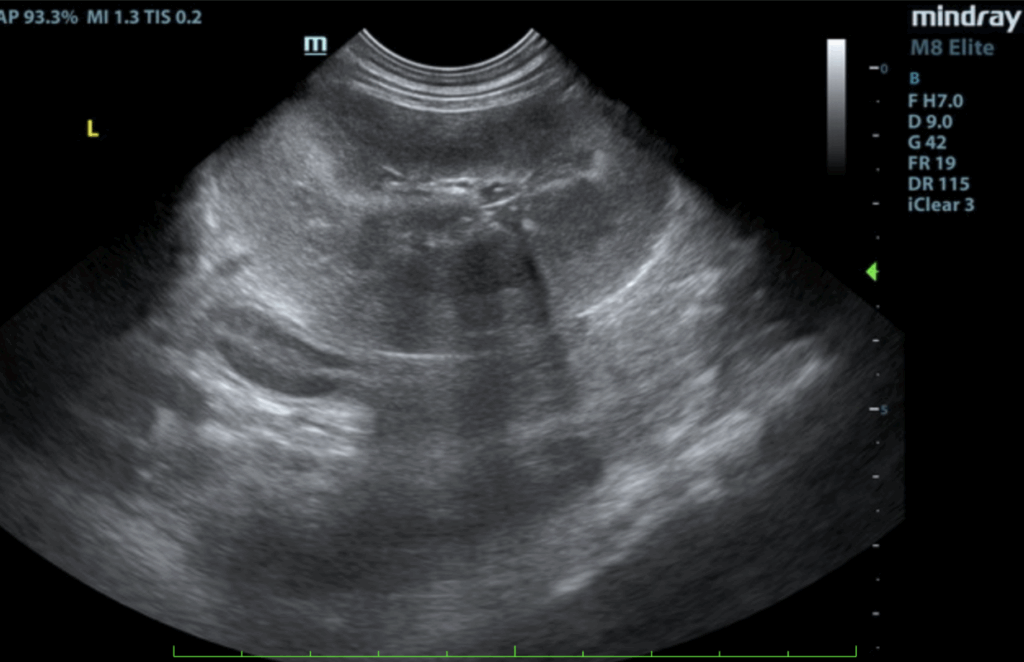
The urinary bladder, trigone, and pelvic urethra presented normal thicknesses and normal tone. The ureters were not visible which is normal. Small calculi were noted, grouping of which measured 1.0 cm. No evidence of inflammatory or neoplastic changes was noted. Ureteral papillae were normal. The kidneys were both swollen and hypervascular. The left kidney measured 6.8 cm. The right kidney measured 7.59 cm.
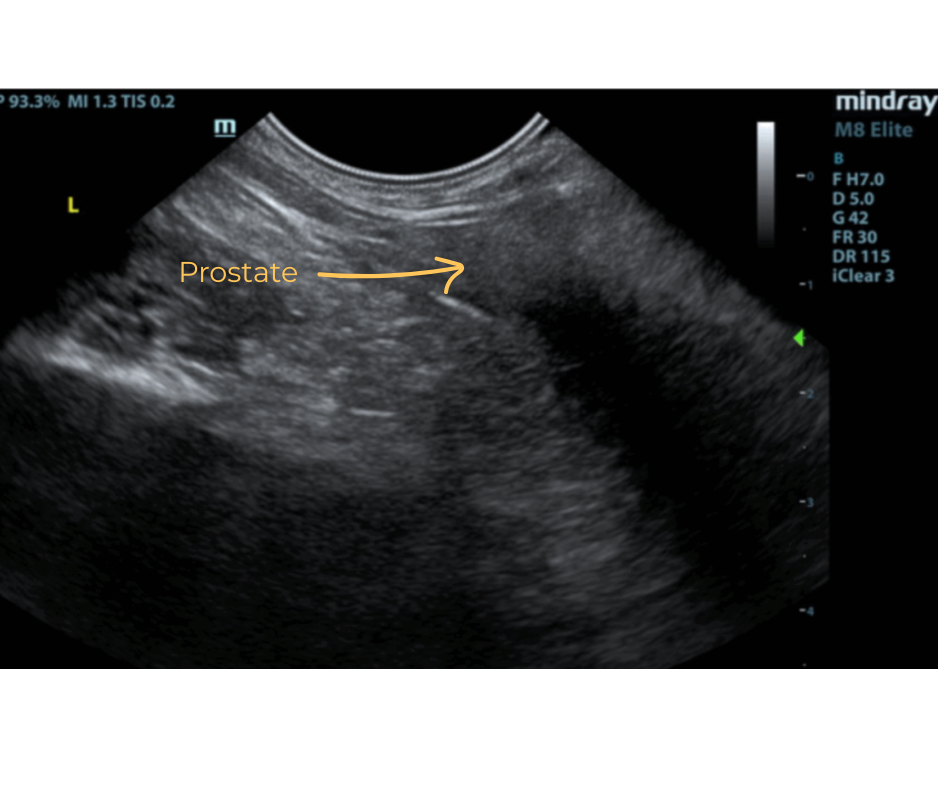
The prostate was uniform and poorly developed measuring 1.0 cm.
The iliac trifurcation was unremarkable.
Adrenal Glands:
Both adrenal glands were visualized and recognized as having normal shape, size, position and echogenicity for this breed. The phrenic vasculature, glandular echogenicity and detail were unremarkable. Capsule, cortex, and medullary definition were normal for this age patient. The right adrenal gland measured 3.19 x 1.01 cm at the cranial pole and 0.62 cm at the caudal pole. The left adrenal gland measured 3.16 x 0.79 cm at the cranial pole and 0.98 cm at the caudal pole.
Spleen:
The spleen presented a smooth homogeneous parenchyma hyperechoic to liver and renal cortical parenchyma. The capsule was smooth without noticeable expansion or deviation from within the spleen or adjacent pathology. The splenic vasculature demonstrated normal volume without signs of congestion or thrombosis. No sonographic evidence of acute or chronic inflammatory, neoplastic, or infarctual changes was noted.
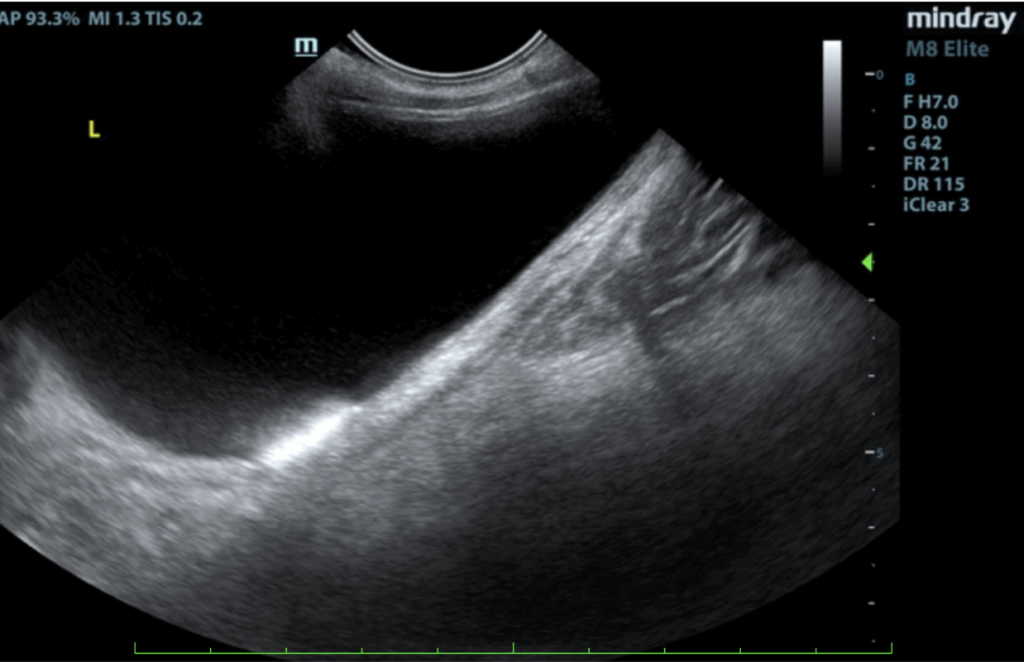
Liver:
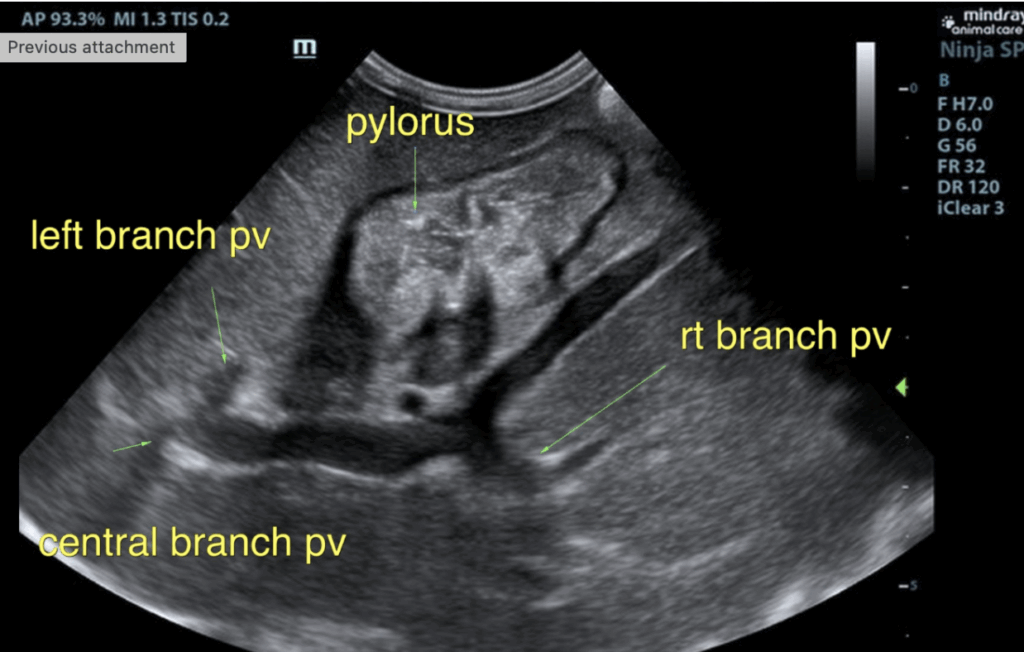
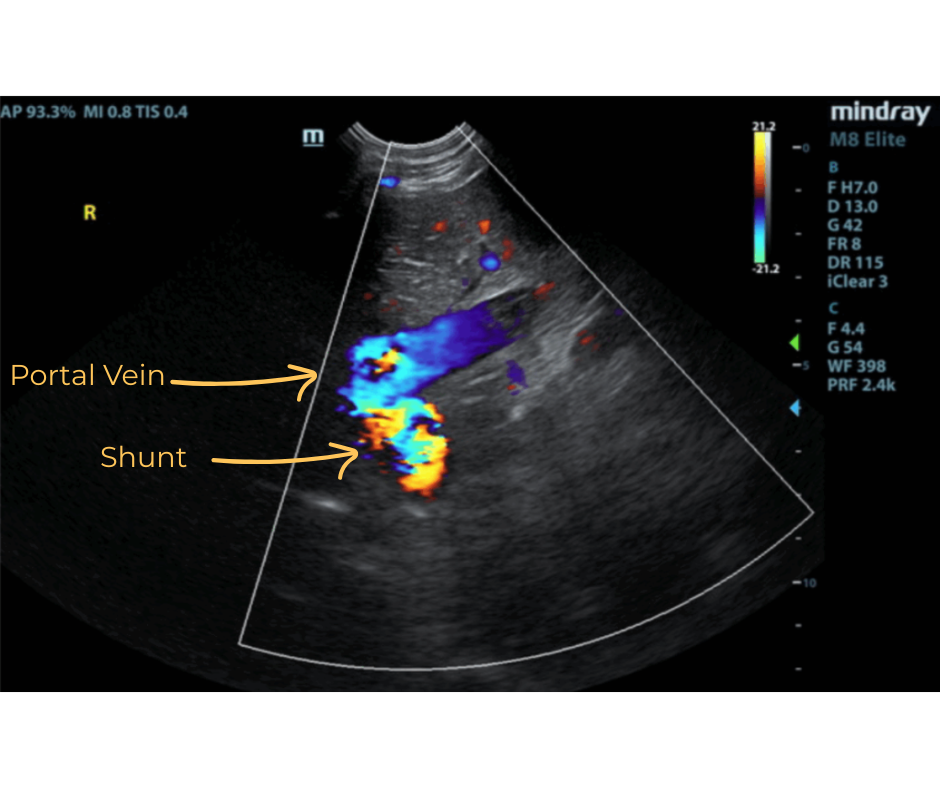
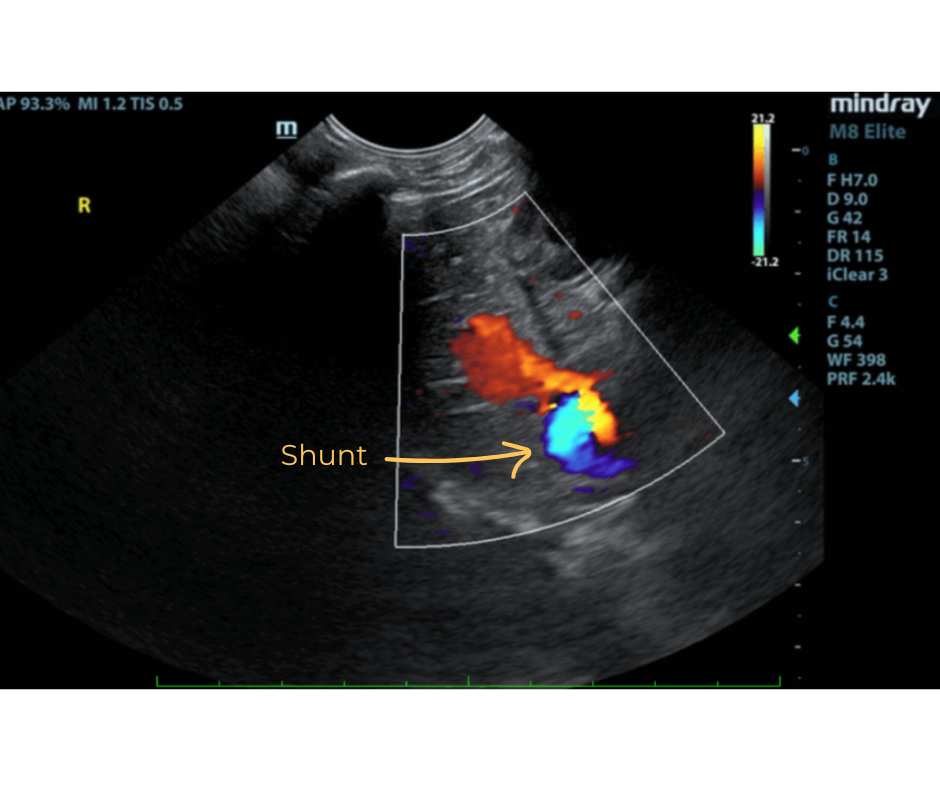
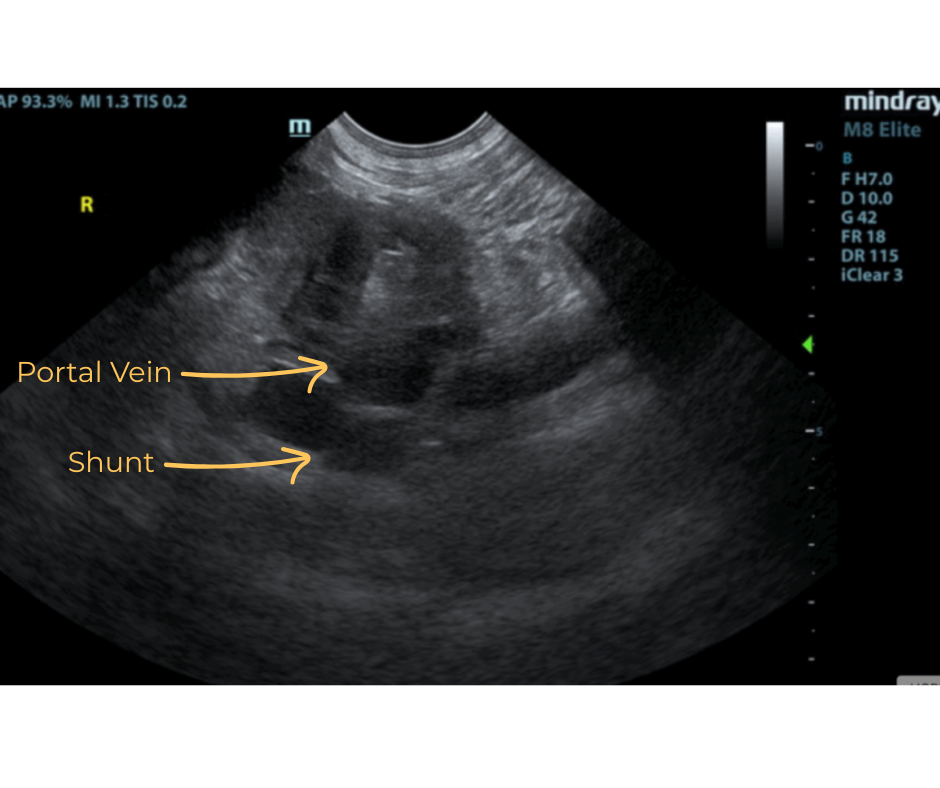
The liver was subnormal in size. The mid dorsal liver in this patient revealed an abnormal intrahepatic branch of the portal vein. This is most consistent with central divisional shunt. However, this should be further evaluated with CT. The gallbladder and common bile duct were unremarkable.
Gastrointestinal:
The stomach revealed a fluid filled lumen and prominent gastric mucosae. Low-grade gastritis is suspected. The small intestines and colon were unremarkable with normal curvilinear mural patterns and content.
Pancreas:
The base and limbs of the pancreas were observed to be largely isoechoic to surrounding omental fat. Pancreatic duct and capsular contour were acceptably normal and parenchyma respected normal curvilinear patterns. No overt evidence of active inflammatory or neoplastic disease was noted.

ULTRASONOGRAPHIC FINDINGS:
- Intrahepatic shunt – suspect central divisional or right divisional shunt
- Swollen kidneys
- Bladder sand
- Poorly developed prostate
INTERPRETATION OF THE FINDINGS & FURTHER RECOMMENDATIONS:
- CT evaluation for confirmation and surgical planning.
Diagnosis:
- Suspected Intrahepatic Shunt
DISCUSSION:
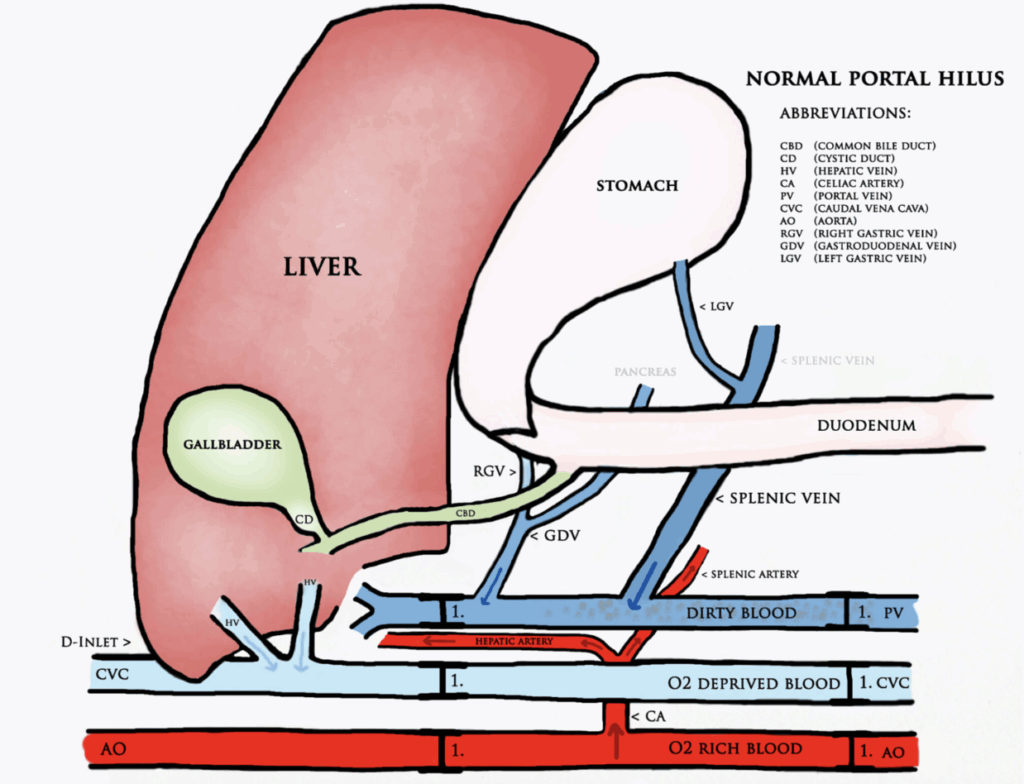
A portosystemic shunt is an abnormal vessel that redirects blood from the portal circulation into the systemic circulation. They are either congenital or acquired, single or multiple, extrahepatic or intrahepatic.
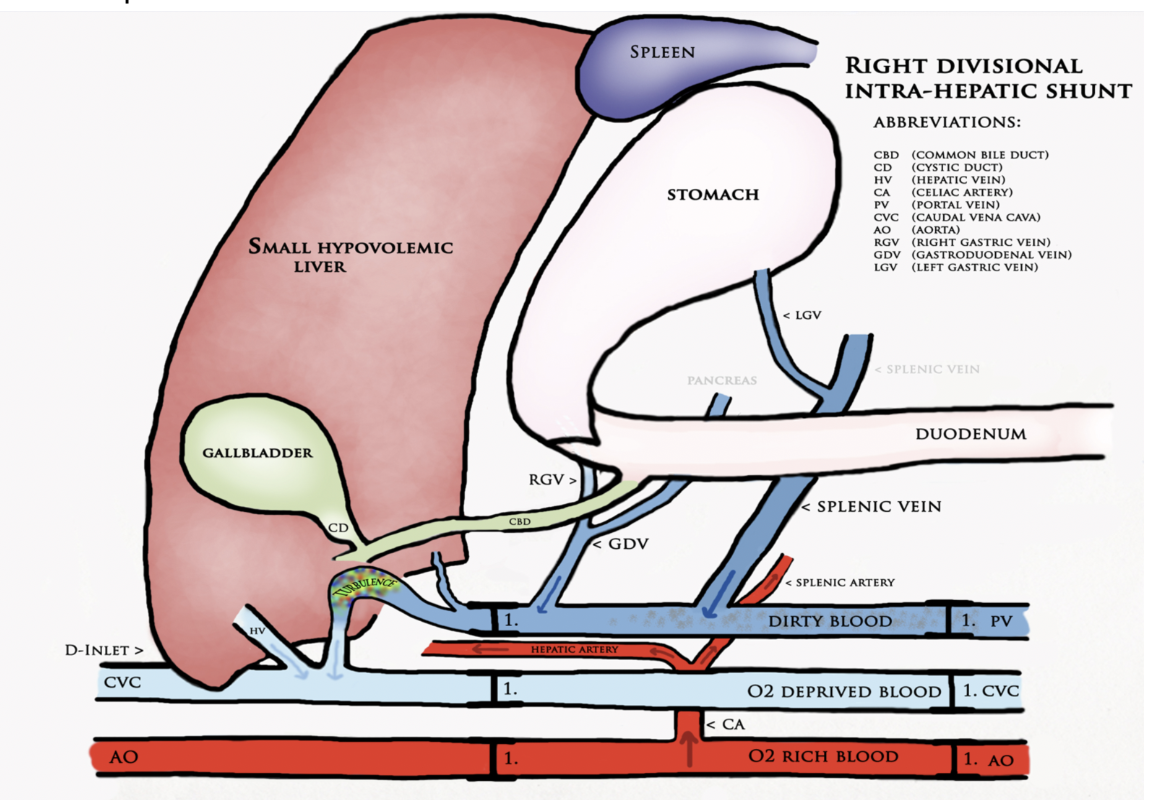
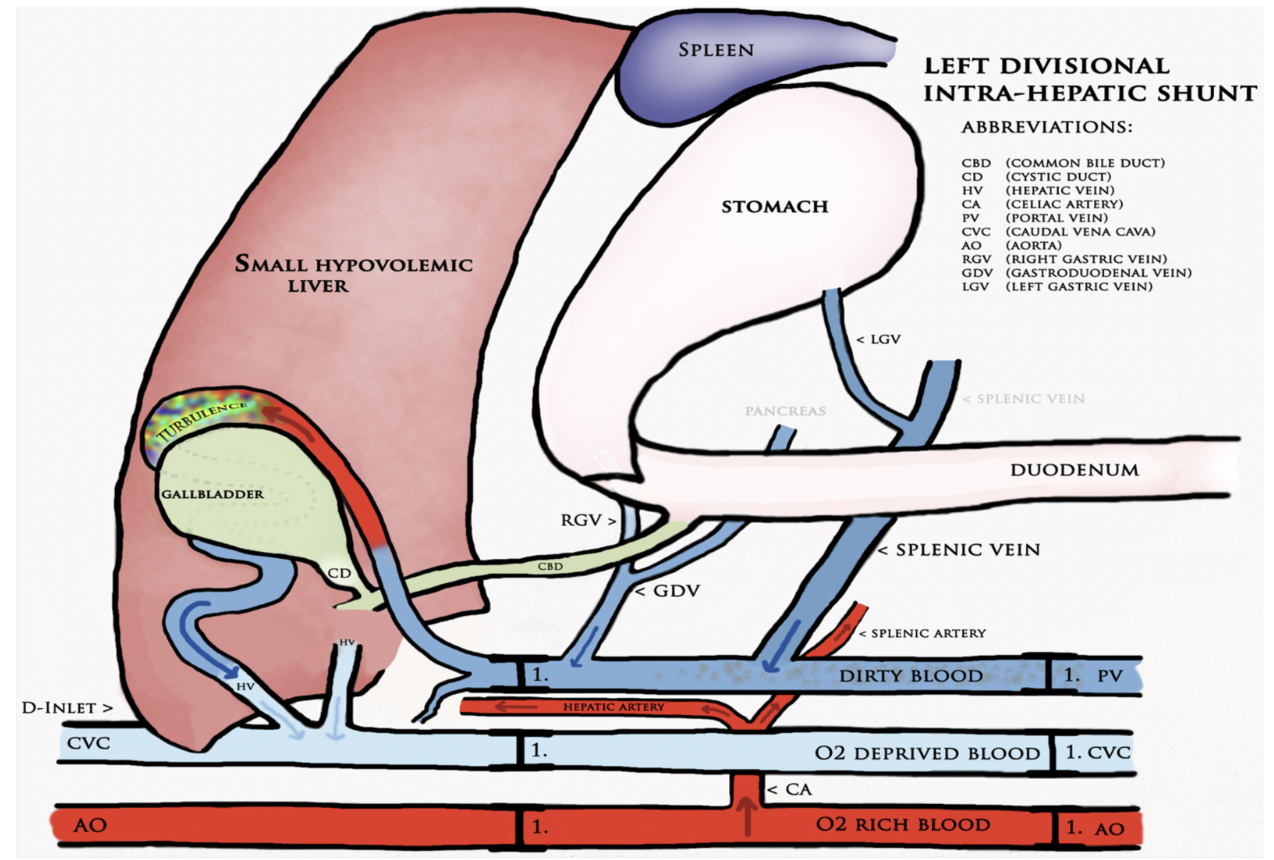
Intrahepatic shunts (IHPSS) are classified as left, central, or right divisional. IHPSS are more commonly seen in large or medium breed dogs.
- Left divisional IHPSS typically form a short connection between the left portal branch and the left hepatic vein and most likely represent a patent ductus venosus.
- Central divisional IHPSS are described as a focal dilation of the portal vein forming a foramen with the caudal vena cava (CVC).
- Right divisional IHPSS involve the right lateral and caudate lobes and form a long loop before connecting to the CVC.
Further studies using CT angiography show even further subclassification of IHPSS inserting into either a hepatic or phrenic vein before inserting into the CVC.
Older studies have shown that the most common type of IHPSS is a left divisional IHPSS. However, a more recent study in 2017 involving 90 dogs showed that a right divisional IHPSS is the most common.
In normal animals, blood from the intestines, pancreas, spleen, and stomach enters the liver through the portal system. This blood contains hormones from the pituitary gland, toxins from the intestines and bacterial products. When an IHPSS exists portal blood bypasses the liver and enters directly into systemic circulation. The liver fails to develop properly, there is decreased protein production, and abnormal fat and protein metabolism. Toxins and byproducts that are usually metabolized or eliminated by the liver then build up in the body. When these reach a certain level hepatic encephalopathy, gastrointestinal signs, poor growth, coagulopathies, and lower urinary tract signs will develop.
Ultrasound can identify a small liver, abnormal vessels, altered portal vein/vena cava ratio, altered portal vein/aorta ratio, renomegaly, and urolithiasis. Identification of an IHPSS with an experienced operator has a sensitivity of 95-100%. IHPSS tend to have a large diameter and they are outlined by the liver parenchyma making them easier to identify. CT scan is used for cases that are unable to be identified using ultrasound and to correctly identify the origin and end point of the shunt for surgical planning.
Conclusion:
The owner was unable to pursue further workup and surgery. The patient was returned to the breeder. The patient was lost to followup and it is unknown if surgical correction of the shunt was performed.
References:
1. Plested MJ, Zwingenberger AL, Brockman DJ, et al. Canine intrahepatic portosystemic shunt insertion into the systemic circulation is commonly through primary hepatic veins as assessed with CT angiography. Veterinary Radiology & Ultrasound 2020;61:519–530.
2. Culp WTN, Zwingenberger AL, Giuffrida MA, et al. Prospective evaluation of outcome of dogs with intrahepatic portosystemic shunts treated via percutaneous transvenous coil embolization. Veterinary Surgery 2018;47:74–85.
3. Konstantinidis AO, Patsikas MN, Papazoglou LG, et al. Congenital Portosystemic Shunts in Dogs and Cats: Classification, Pathophysiology, Clinical Presentation and Diagnosis. Vet Sci 2023;10:160.
4. Parry AT, White RN. Comparison of computed tomographic angiography and intraoperative mesenteric portovenography for extrahepatic portosystemic shunts. Journal of Small Animal Practice 2017;58:49–55.

